Stomach Ulcer Esophagus

The esophagus, stomach, and duodenum are intricately connected components of the gastrointestinal tract, each playing a vital role in the digestion and absorption of nutrients. However, these areas are also prone to various conditions, including stomach ulcers and esophageal disorders, which can significantly impact an individual’s quality of life. Understanding the relationship between stomach ulcers and the esophagus requires a comprehensive look at the anatomy, function, and potential disorders of these regions.
Anatomy and Function of the Esophagus and Stomach
The esophagus is a muscular tube that carries food from the throat to the stomach. It is approximately 10 inches long and is lined with mucous membranes that help facilitate the passage of food. The stomach, a sac-like organ, is responsible for digesting food with the help of gastric acids and enzymes. The stomach lining has several layers, including the mucosa, which produces mucus to protect the stomach from the corrosive effects of gastric acids.
Stomach Ulcers: Definition and Causes
A stomach ulcer, also known as a gastric ulcer, is an open sore that develops on the inside lining of the stomach and the upper portion of the small intestine. The most common symptoms of stomach ulcers include burning stomach pain, vomiting, and difficulty eating. Stomach ulcers are typically caused by an infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of anti-inflammatory drugs like ibuprofen and aspirin, which can irritate and erode the stomach lining.
Esophagus and Stomach Ulcer Connection
While stomach ulcers primarily affect the stomach, they can indirectly influence the functioning and health of the esophagus. For instance, the inflammation and irritation caused by stomach ulcers can lead to an increase in stomach acid production. This excess acid can sometimes flow back into the esophagus, causing heartburn and potentially leading to esophagitis, an inflammation of the esophagus. Additionally, the discomfort and pain associated with stomach ulcers may lead to changes in eating habits or avoidance of certain foods, which can further exacerbate digestive issues, including those affecting the esophagus.
Esophageal Disorders: Impact on Stomach Health
Conversely, disorders of the esophagus can also have implications for stomach health. Gastroesophageal reflux disease (GERD), a condition where stomach acid frequently flows back into the tube connecting the mouth and stomach (esophagus), can lead to inflammation and irritation of the esophagus. Over time, GERD can potentially lead to complications such as esophageal stricture (a narrowing of the esophagus) and Barrett’s esophagus, a condition in which the esophageal lining changes to resemble the lining of the intestine, which can increase the risk of esophageal cancer. The chronic reflux associated with GERD can also put pressure on the stomach, potentially affecting its functioning and contributing to conditions like stomach ulcers.
Management and Treatment
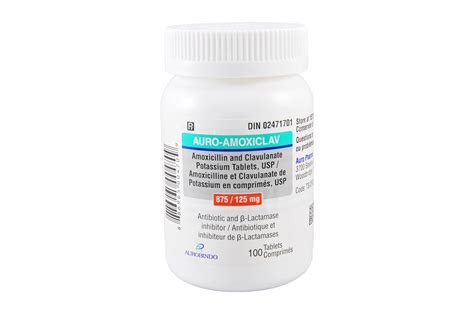
The management and treatment of stomach ulcers and esophageal disorders typically involve a combination of lifestyle modifications, medications, and, in some cases, surgical interventions. For stomach ulcers, treatment often focuses on eliminating the H. pylori infection with antibiotics and reducing acid production in the stomach with medications. Lifestyle changes, such as avoiding spicy or acidic foods, quitting smoking, and reducing alcohol consumption, can also help in managing symptoms and facilitating healing.
For esophageal disorders, particularly GERD, treatment may include antacids or acid reducers to decrease acid production, and in severe cases, surgery to tighten the lower esophageal sphincter or remove damaged portions of the esophagus. Dietary changes, such as eating smaller meals, avoiding trigger foods, and elevating the head of the bed, can help manage symptoms and reduce reflux.
Prevention Strategies
Preventing stomach ulcers and esophageal disorders involves maintaining a healthy lifestyle and being mindful of dietary choices. Eating a balanced diet rich in fruits, vegetables, and whole grains can help reduce the risk of digestive disorders. Avoiding foods that trigger acid reflux, not smoking, limiting alcohol consumption, and maintaining a healthy weight are also important preventive measures. Regular check-ups with a healthcare provider can help in the early detection and management of these conditions, potentially preventing long-term complications.
Advanced Diagnostic Techniques
The diagnosis of stomach ulcers and esophageal disorders has become more precise with the advancement of medical technology. Endoscopy, a procedure where a flexible tube with a camera and light is inserted through the mouth to visualize the inside of the esophagus, stomach, and duodenum, allows for the direct observation of ulcers and other abnormalities. Biopsy samples can be taken during an endoscopy to check for H. pylori infection or precancerous changes in the esophagus. Imaging tests like upper GI series (barium swallow) and CT scans may also be used to evaluate the upper digestive system.
Future Perspectives and Emerging Treatments
Research into the causes and treatments of stomach ulcers and esophageal disorders is ongoing, with a focus on developing more effective therapies and preventive strategies. The role of microbiota in gastrointestinal health is an area of increasing interest, with studies exploring how the manipulation of gut bacteria may help in preventing or treating digestive conditions. Additionally, advancements in surgical techniques, such as minimally invasive surgeries for esophageal disorders, are improving outcomes and reducing recovery times for patients.
Conclusion
Stomach ulcers and esophageal disorders represent significant health challenges that require comprehensive understanding and management strategies. By recognizing the interconnectedness of the stomach and esophagus, individuals can better appreciate the importance of maintaining overall digestive health. Through a combination of medical treatment, lifestyle adjustments, and preventive measures, it is possible to manage and prevent these conditions, improving quality of life and reducing the risk of long-term complications.
What are the common causes of stomach ulcers?
+Stomach ulcers are commonly caused by an infection with the bacterium Helicobacter pylori (H. pylori) and the long-term use of anti-inflammatory drugs like ibuprofen and aspirin.
How can esophageal disorders affect stomach health?
+Esophageal disorders, such as GERD, can lead to an increase in stomach acid production and potentially cause inflammation and irritation of the stomach lining, contributing to conditions like stomach ulcers.
What lifestyle changes can help manage stomach ulcers and esophageal disorders?
+Lifestyle changes such as avoiding spicy or acidic foods, quitting smoking, reducing alcohol consumption, eating smaller meals, and elevating the head of the bed can help manage symptoms and facilitate healing.
How can stomach ulcers and esophageal disorders be prevented?
+Prevention involves maintaining a healthy lifestyle, including eating a balanced diet, avoiding trigger foods, not smoking, limiting alcohol consumption, and maintaining a healthy weight. Regular check-ups with a healthcare provider can also help in early detection and management.
What are the advanced diagnostic techniques for stomach ulcers and esophageal disorders?
+Advanced diagnostic techniques include endoscopy, biopsy, upper GI series (barium swallow), and CT scans, which allow for precise visualization and assessment of the esophagus, stomach, and duodenum.
What does the future hold for the treatment of stomach ulcers and esophageal disorders?
+The future of treatment includes developing more effective therapies, exploring the role of microbiota in digestive health, and advancing surgical techniques to improve patient outcomes and reduce recovery times.