Thoracic Drainage Tube
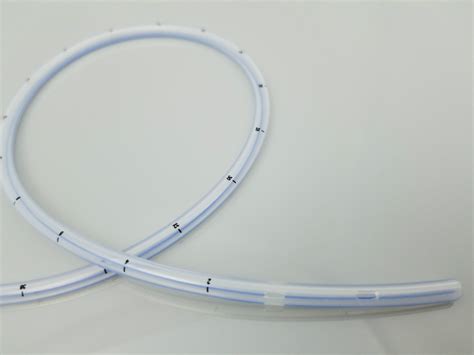
The insertion and management of thoracic drainage tubes, also known as chest tubes, are critical components in the care of patients with a variety of thoracic conditions. These conditions can range from pneumothorax, where air leaks into the space between the lung and chest wall, to pleural effusions, where fluid accumulates in this same space, and other complications that may arise post-surgically or due to trauma.
Indications for Thoracic Drainage
The primary indication for the insertion of a thoracic drainage tube is to evacuate air, fluid, or blood from the pleural space to help the lung re-expand and to restore normal respiratory mechanics. Specific conditions that may necessitate thoracic drainage include:
- Pneumothorax: Air in the pleural space, which can collapse the lung and impair breathing. This can be spontaneous, occurring without apparent cause, or traumatic, resulting from injury.
- Pleural Effusion: Accumulation of fluid in the pleural space, which can be due to infection, malignancy, heart failure, or other causes.
- Hemothorax: Blood in the pleural space, often resulting from trauma.
- Chylothorax: Leakage of lymphatic fluid into the pleural space, which can occur due to injury or blockage of the thoracic duct.
Procedure for Insertion
The insertion of a thoracic drainage tube is typically performed under local anesthesia, although in emergency situations or in certain patient populations (such as pediatric or critically ill patients), general anesthesia or sedation may be used. The procedure involves:
- Preparation: The patient is positioned upright or slightly tilted to facilitate the drainage of fluid or air. The site of insertion is cleaned and disinfected.
- Anesthesia: Local anesthetic is administered to numb the area.
- Incision and Insertion: A small incision is made in the skin, and the thoracic drainage tube is inserted into the pleural space using a trocar or a blunt dissection technique.
- Connection to Drainage System: The tube is then connected to a drainage system, which may include a collection chamber for fluid, a water seal chamber to prevent air from re-entering the pleural space, and possibly a suction control chamber to apply negative pressure to facilitate drainage.
Management and Care
Proper management and care of the thoracic drainage tube are essential to ensure effective drainage, prevent complications, and promote patient comfort. Key aspects include:
- Monitoring: Regular inspection of the drainage system for air leaks, fluid drainage, and evidence of tube blockage or kinking.
- Drainage Record: Accurate recording of the amount and character of drainage.
- Pain Management: Adequate pain control measures to manage discomfort associated with the tube.
- Mobility: Encouraging patient mobility to prevent complications such as pneumonia and deep vein thrombosis.
- Infection Control: Strict adherence to sterile technique during insertion and subsequent care to prevent infection.
Complications
Despite the lifesaving potential of thoracic drainage tubes, their insertion and management are not without potential complications. These can include:
- Bleeding or Hemorrhage: From the intercostal vessels or from injury to major vessels.
- Infection: Either at the site of insertion or within the pleural space.
- Lung Injury: Including laceration of the lung tissue.
- Re-expansion Pulmonary Edema: A rare but serious complication that occurs when the lung expands too quickly after a long period of collapse.
Conclusion
Thoracic drainage tubes are a vital tool in the management of thoracic conditions, offering a means to restore normal respiratory function and alleviate the distressing symptoms associated with pneumothorax, pleural effusions, and other conditions. Their effective insertion and management require a deep understanding of thoracic anatomy, the indications for their use, the procedural techniques involved, and the complications that can arise. As medical practice continues to evolve, the role of thoracic drainage tubes will remain central to the care of patients with thoracic disease, underscoring the importance of ongoing education and training for healthcare professionals involved in their insertion and management.
What are the most common complications associated with thoracic drainage tubes?
+The most common complications include bleeding or hemorrhage, infection at the site of insertion or within the pleural space, lung injury, and re-expansion pulmonary edema. These complications can be minimized with proper technique, meticulous care, and close monitoring of the patient.
How are thoracic drainage tubes managed post-insertion to prevent complications?
+Post-insertion management includes regular monitoring of the drainage system for air leaks and blockages, maintaining an accurate record of fluid drainage, ensuring proper pain management, promoting patient mobility, and adhering to strict infection control measures. Regular inspections and maintenance of the drainage system are also crucial.
What are the indications for the removal of a thoracic drainage tube?
+Indications for removal include resolution of the condition for which the tube was inserted (e.g., full expansion of the lung in pneumothorax, drainage of effusion), minimal or no air leak for a specified period, and when the volume of drainage significantly decreases, suggesting that the tube is no longer necessary. The decision to remove the tube should be made based on clinical judgment and may involve chest radiography to confirm tube placement and lung expansion.