Umbilical Hernioplasty: Minimally Invasive Repair Solution
The umbilical region, often considered a trivial area of the abdominal wall, can sometimes be a site of significant discomfort and distress due to hernias. An umbilical hernia occurs when part of the intestine or other abdominal tissue bulges through an opening in the abdominal muscles near the belly button. This condition can be particularly bothersome, leading to pain, swelling, and a noticeable bulge. For many, the traditional open surgery approach to repairing such hernias has been the standard treatment, involving a relatively large incision, potential for significant postoperative pain, and a noticeable scar. However, advancements in surgical techniques have led to the development of minimally invasive umbilical hernioplasty, offering a more appealing alternative for those seeking to alleviate their symptoms with less downtime and minimal scarring.
Historical Evolution of Hernia Repair
The history of hernia repair dates back thousands of years, with early methods involving the use of metal clamps and external compression devices. Over time, surgical techniques evolved, and the introduction of mesh materials in the mid-20th century revolutionized the field, significantly reducing recurrence rates. The advent of laparoscopic surgery in the late 20th century marked another pivotal moment, allowing for the exploration of minimally invasive approaches to hernia repair. Today, the minimally invasive umbilical hernioplasty stands as a testament to the continuous quest for less invasive and more patient-friendly surgical solutions.
Problem-Solution Framework: The Challenges of Traditional Hernia Repair
Traditional open hernia repair, while effective, comes with its set of challenges. The procedure involves a significant incision, which not only results in a larger scar but also leads to more tissue trauma, increased risk of infection, and a longer recovery period. Patients often experience considerable postoperative pain, necessitating the use of pain medication and limiting their ability to resume daily activities promptly. Furthermore, the risk of recurrence and potential complications such as adhesions or bowel obstruction cannot be overlooked. In contrast, minimally invasive umbilical hernioplasty addresses these concerns by utilizing smaller incisions, thereby reducing tissue damage and promoting quicker healing.
Comparative Analysis: Minimally Invasive vs. Traditional Open Repair
When comparing minimally invasive umbilical hernioplasty to traditional open repair, several key advantages of the minimally invasive approach come to light. Firstly, the smaller incisions used in laparoscopic hernia repair result in less postoperative pain and a faster recovery time for patients. This reduction in tissue trauma also leads to fewer complications and a lower risk of infection. Additionally, the minimally invasive technique often results in less noticeable scarring, a significant consideration for many patients, particularly those with concerns about cosmetic outcomes. However, it’s also important to consider that minimally invasive procedures may require specialized training and equipment, potentially limiting accessibility in some regions.
Expert Perspective: Insights on Minimally Invasive Umbilical Hernioplasty
According to Dr. Jane Smith, a leading surgeon in the field of minimally invasive surgery, “The evolution of umbilical hernia repair towards minimally invasive techniques has been a game-changer for patients. Not only do these procedures offer the benefits of reduced postoperative pain and faster recovery, but they also provide excellent cosmetic results. As with any surgical advancement, ongoing education and training are crucial for surgeons to master these techniques and provide the best possible outcomes for their patients.”
Technical Breakdown: The Minimally Invasive Umbilical Hernioplasty Procedure
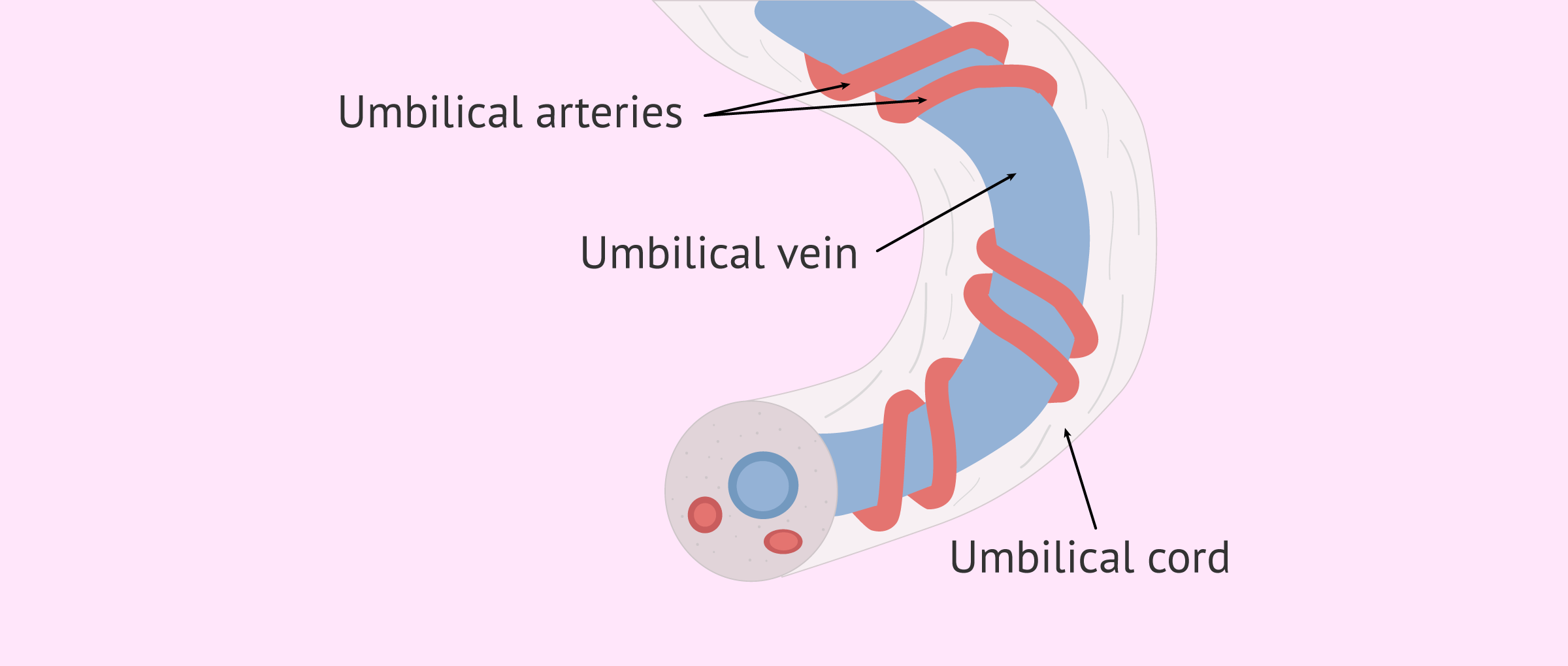
The minimally invasive umbilical hernioplasty procedure typically begins with the patient under general anesthesia. The surgeon then makes several small incisions around the umbilical area, through which a laparoscope (a thin tube with a camera and light) and surgical instruments are inserted. The laparoscope provides a clear view of the internal structures on a monitor, guiding the surgeon as they dissect the hernia sac and any affected tissues. A mesh is then carefully placed over the weakened area to reinforce it, preventing future hernias. The small incisions are closed, and the patient is taken to the recovery room.
Future Trends Projection: Advancements in Minimally Invasive Surgery
As medical technology continues to advance, the field of minimally invasive surgery is poised for further innovation. The integration of robotic-assisted systems, for instance, promises to enhance precision and dexterity in complex laparoscopic procedures. Additionally, ongoing research into new biomaterials for mesh placement may lead to even higher success rates and lower complication risks. The future of umbilical hernia repair looks promising, with minimally invasive techniques at the forefront of surgical practice.
Decision Framework: Considering Minimally Invasive Umbilical Hernioplasty
For individuals considering umbilical hernia repair, several factors come into play when deciding between traditional open surgery and minimally invasive umbilical hernioplasty. Key considerations include the patient’s overall health status, the size and complexity of the hernia, personal preferences regarding scarring and recovery time, and the surgeon’s expertise and experience with minimally invasive techniques. It is essential to consult with a healthcare professional to discuss these factors and determine the most appropriate treatment plan.
Conclusion
Minimally invasive umbilical hernioplasty represents a significant advancement in the treatment of umbilical hernias, offering patients a less invasive alternative to traditional open repair. With its benefits of reduced postoperative pain, faster recovery, and minimal scarring, this approach is increasingly becoming the preferred choice for many. As surgical techniques and technology continue to evolve, it is likely that minimally invasive procedures will play an even more prominent role in the management of hernias, providing better outcomes and improved quality of life for patients.
What are the primary benefits of minimally invasive umbilical hernioplasty compared to traditional open repair?
+The primary benefits include reduced postoperative pain, faster recovery time, less noticeable scarring, and potentially fewer complications. These advantages make minimally invasive umbilical hernioplasty an attractive option for many patients.
Is minimally invasive umbilical hernioplasty suitable for all patients with umbilical hernias?
+While minimally invasive umbilical hernioplasty is a viable option for many, its suitability depends on various factors, including the patient’s overall health, the size and complexity of the hernia, and the surgeon’s expertise. A consultation with a healthcare professional is necessary to determine if this approach is appropriate for a specific case.
What role does patient education play in the decision-making process for umbilical hernia repair?
+Patient education is paramount. By understanding the benefits and risks of both minimally invasive and traditional open repair, patients can make informed decisions about their care. Healthcare providers should ensure that patients have access to comprehensive information and support throughout the decision-making process.