What Are Normal Bg Levels? Stable Control Tips
Maintaining normal blood glucose (BG) levels is crucial for overall health, particularly for individuals with diabetes. Blood glucose levels fluctuate throughout the day due to various factors such as diet, physical activity, and medication. Understanding what constitutes normal BG levels and how to achieve stable control is essential for managing diabetes effectively and preventing complications.
Normal Blood Glucose Levels
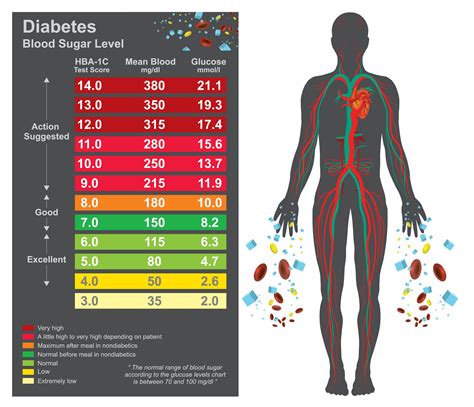
Normal blood glucose levels vary throughout the day, with the following values generally considered within the target range for individuals without diabetes: - Fasting glucose: Less than 100 mg/dL (5.6 mmol/L) - 1-2 hours after meals: Less than 140 mg/dL (7.8 mmol/L)
For individuals with diabetes, the American Diabetes Association (ADA) recommends the following target blood glucose levels: - Fasting: 80-130 mg/dL (4.4-7.2 mmol/L) - Before meals: 70-130 mg/dL (3.9-7.2 mmol/L) - 1-2 hours after meals: Less than 180 mg/dL (10.0 mmol/L)
Tips for Stable Blood Glucose Control
Achieving stable blood glucose control requires a multifaceted approach that includes dietary management, physical activity, monitoring, and medication (if prescribed). Here are several tips to help maintain stable BG levels:
Balanced Diet: Eating a balanced diet that is low in added sugars, saturated fats, and sodium can help stabilize blood glucose levels. Focus on whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats.
Carb Counting: For individuals with diabetes, understanding how different carbohydrate sources affect blood glucose levels is crucial. Carb counting can help manage post-meal spikes by balancing carbohydrate intake with insulin doses or physical activity.
Regular Physical Activity: Exercise helps the body use insulin more efficiently and can lower blood glucose levels. Aim for at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week. Additionally, include strength-training activities at least twice a week.
Stay Hydrated: Drinking enough water can help the body regulate blood glucose levels and prevent dehydration, a complication of high blood sugar.
Regulate Stress: Stress can raise blood glucose levels. Engage in stress-reducing techniques like yoga, meditation, or deep breathing exercises.
Monitor Blood Glucose Regularly: Regular monitoring can help identify patterns and fluctuations in blood glucose levels, allowing for timely adjustments to diet, exercise, or medication.
Medication Adherence: If prescribed medication or insulin, take it as directed. Consult with your healthcare provider before making any changes to your medication regimen.
Adequate Sleep: Lack of sleep can disrupt the balance of hormones that regulate glucose metabolism, leading to higher blood glucose levels. Aim for 7-8 hours of sleep per night.
Limit Alcohol: Alcohol can cause blood glucose levels to rise or fall, depending on the amount consumed. Limit alcohol intake to moderate levels (up to one drink a day for women and up to two drinks a day for men).
Regular Health Check-Ups: Regular visits to your healthcare provider can help monitor the progression of diabetes, adjust treatment plans as necessary, and prevent complications.
Managing Blood Glucose Levels: A Long-Term Commitment
Managing blood glucose levels is a long-term commitment that requires patience, persistence, and the right strategies. By understanding normal BG levels and implementing stable control tips, individuals can effectively manage their condition, reduce the risk of complications, and improve their quality of life.
Future Trends and Emerging Technologies
The management of diabetes and blood glucose levels is an area of ongoing research, with emerging technologies and trends promising to further simplify and personalize care. These include: - Continuous Glucose Monitors (CGMs): Devices that track glucose levels throughout the day and night, providing real-time data to help manage blood sugar spikes and dips. - Artificial Pancreas Systems: Automated systems that use CGM data and insulin pumps to automatically adjust insulin doses. - Personalized Nutrition and Diabetes Management: Tailored dietary advice and treatment plans based on an individual’s genetic profile, lifestyle, and health status.
Conclusion
Maintaining normal blood glucose levels is a multifaceted challenge that requires a comprehensive approach, including dietary adjustments, regular physical activity, monitoring, and adherence to medication regimens. By staying informed about normal BG levels, implementing stable control strategies, and leveraging emerging technologies, individuals with diabetes can achieve better blood glucose control, reduce the risk of complications, and enhance their overall well-being.
FAQ Section
What are the normal blood glucose levels for individuals without diabetes?
+Normal blood glucose levels for individuals without diabetes are typically less than 100 mg/dL (5.6 mmol/L) when fasting and less than 140 mg/dL (7.8 mmol/L) 1-2 hours after meals.
How often should I monitor my blood glucose levels if I have diabetes?
+The frequency of monitoring blood glucose levels varies based on the type of diabetes, treatment plan, and individual needs. Generally, individuals with diabetes should monitor their levels at least four times a day, including before meals and before bedtime, but the specific schedule should be determined in consultation with a healthcare provider.
What role does diet play in managing blood glucose levels?
+Diet plays a crucial role in managing blood glucose levels. A balanced diet that is low in added sugars, saturated fats, and sodium, and rich in whole foods like vegetables, fruits, whole grains, lean proteins, and healthy fats can help stabilize blood glucose levels.