What Is A Beta Blocker
Beta blockers, also known as beta-adrenergic blocking agents, are a class of medications that play a crucial role in managing various health conditions, particularly those related to the cardiovascular system. At their core, beta blockers work by inhibiting the effects of the hormone epinephrine, also known as adrenaline, and by slowing the heart rate and reducing its workload. This mechanism of action has far-reaching implications for patients suffering from conditions such as hypertension, angina, heart failure, and arrhythmias, among others.
Historical Evolution of Beta Blockers
The development of beta blockers is a fascinating story that reflects the evolving understanding of the human body’s physiological responses to stress and the impact of epinephrine on the heart. The first beta blocker, pronethalol, was synthesized in the late 1950s, but its clinical use was limited due to side effects. The breakthrough came with the introduction of propranolol in the early 1960s, which marked the beginning of a new era in the treatment of cardiovascular diseases. Since then, numerous beta blockers have been developed, each with its unique properties and applications.
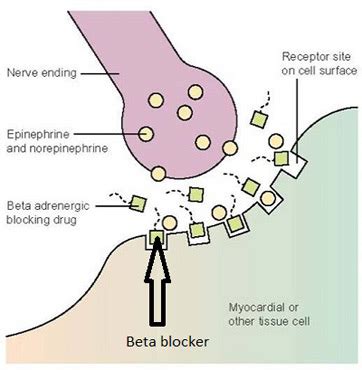
How Beta Blockers Work
To comprehend the effectiveness of beta blockers, it’s essential to understand their interaction with the body’s beta receptors. These receptors are found in various tissues, including the heart, where they regulate heart rate and contractility. When epinephrine binds to these receptors, it typically increases heart rate and the force of heart contractions, preparing the body for ‘fight or flight.’ Beta blockers interfere with this process by blocking the beta receptors, thereby reducing the heart rate, the force of contraction, and ultimately, the heart’s demand for oxygen. This reduction in cardiac workload is particularly beneficial for patients with heart conditions, as it can help alleviate symptoms and improve survival rates.
Types of Beta Blockers
Beta blockers are not a homogeneous group; they vary significantly in their selectivity for beta-1 versus beta-2 receptors, their pharmacokinetic properties, and their intrinsic sympathomimetic activity (ISA). Beta-1 selective blockers, such as atenolol and metoprolol, predominantly affect the heart, making them preferred choices for patients with certain respiratory conditions. Non-selective beta blockers, like propranolol, affect both beta-1 and beta-2 receptors, which can lead to more pronounced effects on the airways and peripheral circulation. The choice of beta blocker depends on the patient’s specific condition, other health issues, and potential side effects.
Clinical Applications of Beta Blockers
The therapeutic applications of beta blockers are diverse and well-documented. In the context of hypertension, beta blockers help reduce blood pressure by decreasing cardiac output and promoting vasodilation. For patients with angina, beta blockers decrease the frequency of angina attacks by reducing myocardial oxygen demand. In heart failure, beta blockers have been shown to improve survival and reduce hospitalizations by counteracting the harmful effects of chronic sympathetic activation. Additionally, beta blockers are used to manage arrhythmias, prevent migraines, and treat performance anxiety.
Potential Side Effects and Considerations
While beta blockers are effective and generally well-tolerated, they can cause side effects that range from mild to severe. Common side effects include fatigue, dizziness, and bradycardia (slow heart rate). Less frequently, beta blockers can exacerbate asthma or COPD in susceptible individuals due to their bronchoconstrictive effects on the airways. Given their potential to mask hypoglycemic symptoms and impair glucose tolerance, beta blockers require careful consideration in diabetic patients. Furthermore, abrupt discontinuation of beta blockers can lead to rebound tachycardia or even myocardial infarction, emphasizing the importance of gradual tapering under medical supervision.
Future Trends and Developments
As our understanding of cardiovascular diseases evolves, so too does the role of beta blockers in their management. Ongoing research focuses on developing beta blockers with improved selectivity and fewer side effects. The integration of beta blockers into combination therapies, such as those including ACE inhibitors or ARBs for heart failure, represents a promising approach to enhancing patient outcomes. Moreover, the increasing recognition of the interplay between the cardiovascular system and other bodily systems, such as the renal and nervous systems, underscores the potential for beta blockers to play a role in managing complex, multimorbid conditions.
Decision Framework for Prescribing Beta Blockers
The decision to prescribe beta blockers involves a nuanced consideration of the patient’s clinical profile, including the nature and severity of their condition, comorbidities, and potential for drug interactions. A step-by-step approach may include:
- Assessing Indications: Evaluate the patient’s condition to determine if beta blockers are appropriate.
- Selecting the Right Beta Blocker: Choose a beta blocker based on its pharmacological properties and the patient’s specific needs.
- Initiating Therapy: Start with a low dose and gradually increase as necessary and tolerated.
- Monitoring: Regularly monitor the patient for efficacy and side effects, adjusting the dose or switching to a different beta blocker as needed.
- Education: Inform the patient about the benefits, potential side effects, and the importance of adherence to the prescribed regimen.
Conclusion
Beta blockers are a cornerstone in the management of various cardiovascular conditions, offering a well-established and effective approach to reducing morbidity and mortality. Their ability to mitigate the effects of epinephrine on the heart, coupled with their relatively favorable side effect profile, makes them an indispensable tool in clinical practice. As medical science continues to evolve, the strategic use of beta blockers, either alone or in combination with other therapies, will remain a critical component of cardiovascular care.
FAQ Section
What are the primary uses of beta blockers in clinical practice?
+Beta blockers are primarily used to manage conditions such as hypertension, angina, heart failure, and arrhythmias. They work by reducing the heart rate and the force of heart contractions, which can help alleviate symptoms and improve survival rates in patients with these conditions.
Can beta blockers be used in patients with asthma or COPD?
+Beta blockers should be used with caution in patients with asthma or COPD, as they can cause bronchoconstriction. However, beta-1 selective blockers may be safer options for these patients compared to non-selective beta blockers. It’s crucial to weigh the benefits against the risks under the guidance of a healthcare provider.
How should beta blockers be discontinued to avoid rebound effects?
+To avoid rebound tachycardia or worsening of angina, beta blockers should be tapered off gradually over a period of weeks under medical supervision. Abrupt cessation is not recommended, as it can lead to severe cardiac complications.
Can beta blockers be used during pregnancy?
+The use of beta blockers during pregnancy should be carefully considered, balancing the benefits of therapy against potential fetal risks. Some beta blockers are safer than others, and the decision to use them should be made in consultation with a healthcare provider, taking into account the specific circumstances of the pregnancy.
How do beta blockers interact with other medications?
+Beta blockers can interact with a variety of medications, including other cardiovascular drugs, and these interactions can either enhance or diminish their effects. It’s essential for patients to inform their healthcare providers about all medications they are taking to minimize potential interactions and ensure safe use.



