What Meds Work For Prediabetes? Natural Solutions
For individuals dealing with prediabetes, the primary goal is to prevent the onset of type 2 diabetes through lifestyle modifications and, in some cases, medication. While there are several medications that can help manage blood sugar levels, it’s also important to consider natural solutions that can be effective in conjunction with or sometimes even instead of pharmaceuticals. Let’s delve into both the medical and natural approaches to managing prediabetes.
Medical Approaches
Several medications are used to treat prediabetes, aiming to reduce blood glucose levels and improve insulin sensitivity. These include:
Metformin: This is often the first-line treatment for prediabetes, especially for those who are overweight or have a history of gestational diabetes. Metformin works by decreasing glucose production in the liver, improving the body’s sensitivity to insulin, and thereby facilitating the uptake of glucose by cells.
Acarbose: This drug delays carbohydrate absorption in the gut, reducing the rise in blood glucose levels after meals. However, it can cause gastrointestinal side effects like bloating, gas, and diarrhea.
Thiazolidinediones (TZDs): These medications increase insulin sensitivity, making it easier for glucose to enter cells. However, they can have significant side effects, including an increased risk of heart failure and bone fractures, which limits their use.
GLP-1 Receptor Agonists: These are typically used for type 2 diabetes but can be considered in some cases of prediabetes. They mimic a natural hormone that helps lower postprandial glucose levels.
Natural Solutions
While medications can be effective, natural solutions offer a holistic approach to managing prediabetes without the risk of pharmaceutical side effects. The cornerstone of natural management includes:
Dietary Changes: Adopting a diet rich in whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats can significantly improve insulin sensitivity and reduce blood glucose levels. Specific diets, such as the Mediterranean Diet or the DASH Diet, have been shown to be effective.
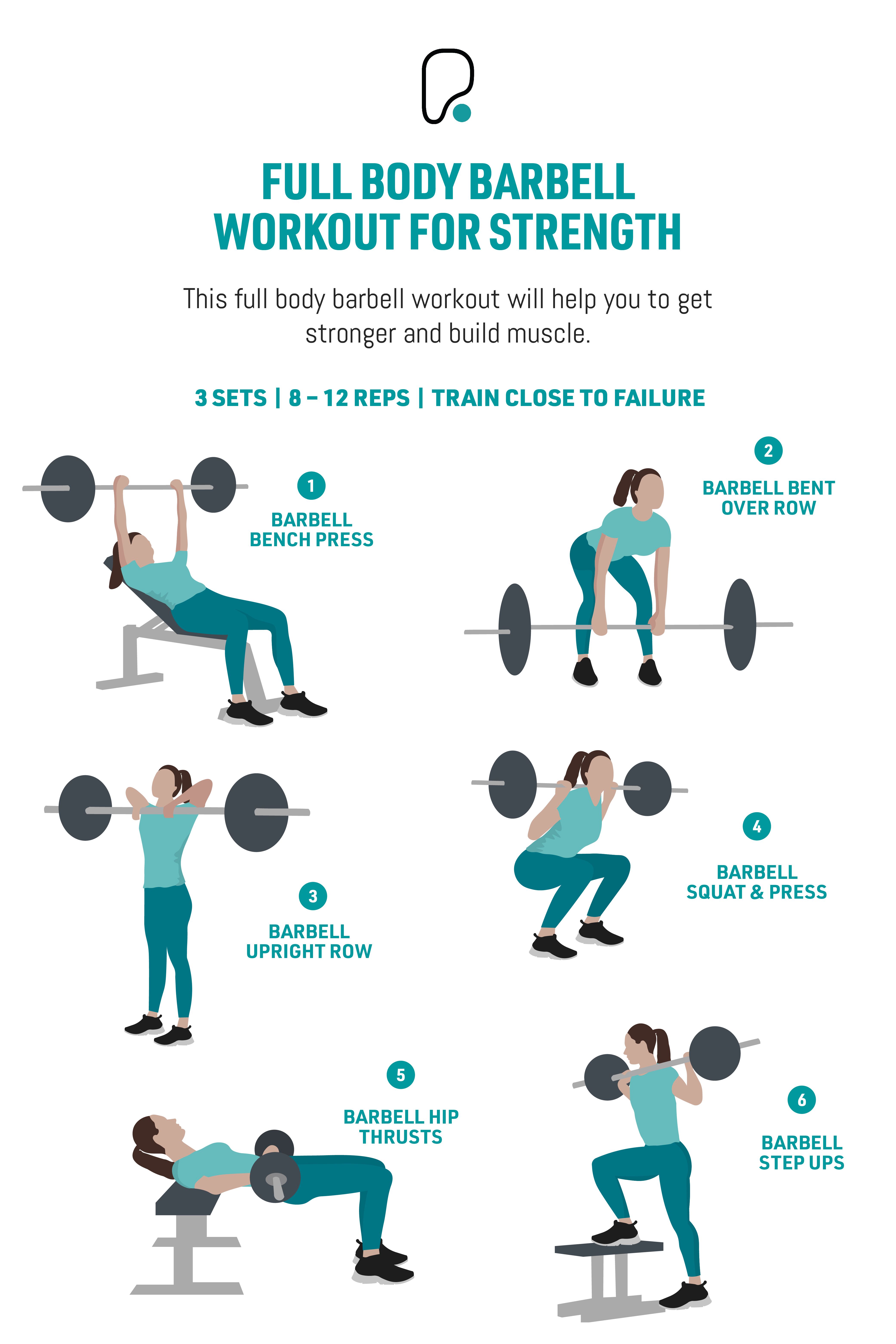
Physical Activity: Regular exercise, including both aerobic workouts and strength training, can enhance insulin sensitivity, reduce body fat, and improve overall health. Aim for at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week, along with muscle-strengthening activities on two or more days.
Weight Loss: For those who are overweight or obese, losing even a small amount of weight (5-10% of initial body weight) can improve insulin sensitivity and reduce the risk of progressing to type 2 diabetes.
Stress Management: Chronic stress can elevate cortisol levels, which can contribute to insulin resistance. Practices like yoga, meditation, and deep breathing exercises can help manage stress levels.
Sleep: Ensuring adequate sleep (7-8 hours for most adults) is crucial, as sleep deprivation can lead to increased insulin resistance and higher glucose levels.
Supplements and Herbs: Certain natural supplements, such as berberine, chromium, and magnesium, have been studied for their potential in improving insulin sensitivity and reducing blood glucose levels. However, it’s essential to consult with a healthcare provider before starting any supplements, as they can interact with medications or have adverse effects in certain individuals.
Implementation and Monitoring
When adopting natural solutions or starting medications, it’s crucial to work closely with a healthcare provider. They can help monitor progress, adjust treatment plans as necessary, and ensure that any changes are safe and effective. Regular check-ups should include measurements of blood glucose levels (fasting and postprandial), HbA1c levels, blood pressure, lipid profiles, and body weight.
Conclusion
Managing prediabetes effectively requires a comprehensive approach that may include medications, lifestyle modifications, and natural solutions. By understanding the options available and working with healthcare professionals, individuals can make informed decisions about their care, reduce their risk of developing type 2 diabetes, and improve their overall well-being.
FAQ Section
What are the primary dietary recommendations for managing prediabetes?
+Focusing on whole, unprocessed foods such as vegetables, fruits, whole grains, lean proteins, and healthy fats. Avoid sugary drinks, refined carbohydrates, and saturated fats.
Can exercise alone reverse prediabetes?
+While exercise is a crucial component of managing prediabetes, it is often most effective when combined with dietary changes and, if necessary, weight loss. Exercise can improve insulin sensitivity, but the overall lifestyle approach determines the outcome.
How often should I monitor my blood glucose levels if I have prediabetes?
+Monitoring frequency can vary based on individual health status and the specific recommendations of your healthcare provider. Typically, checking fasting glucose levels and occasionally after meals can provide valuable insights into how your body is responding to dietary and lifestyle changes.
Each person’s journey with prediabetes is unique, and what works for one individual may not work for another. By exploring both medical and natural solutions under the guidance of a healthcare professional, individuals can find the most effective approach for their specific needs and work towards a healthier future.