Yeast Infection Before Period: Causes & Cures

The delicate balance of the female reproductive system can sometimes be disrupted, leading to uncomfortable and frustrating issues like yeast infections. For many women, the timing of these infections can seem mystifying, often appearing to coincide with their menstrual cycle. One common phenomenon reported by women is experiencing a yeast infection before their period. But what are the causes behind this peculiar timing, and more importantly, what can be done to cure and prevent these infections?
To understand why yeast infections might occur more frequently or severely before a period, it’s essential to delve into the interplay between hormonal changes, the immune system, and the natural flora of the vagina. Normally, the vagina hosts a balance of different microorganisms, with Lactobacillus bacteria being predominant. These beneficial bacteria help maintain an acidic environment, which is less favorable for the overgrowth of Candida, a type of fungus that causes yeast infections. However, the balance can be tipped by various factors, especially the fluctuations in estrogen levels that occur throughout the menstrual cycle.
Hormonal Changes and Yeast Infections
Estrogen levels rise during the first half of the menstrual cycle, reaching a peak right before ovulation. This surge can promote the growth of Candida by increasing the glycogen content in the vagina, which Candida can use as a food source. Furthermore, the week preceding menstruation is marked by a decline in estrogen levels, coupled with an increase in progesterone. This shift can affect the vaginal mucosa and potentially alter the local immune response, making it harder for the body to control Candida growth.
Other Contributing Factors
While hormonal changes provide a plausible explanation for the timing of yeast infections in relation to the menstrual cycle, other factors can contribute to the susceptibility and severity of these infections:
- Immune System Suppression: Stress, lack of sleep, and overall health can impact the immune system’s efficiency in keeping Candida under control.
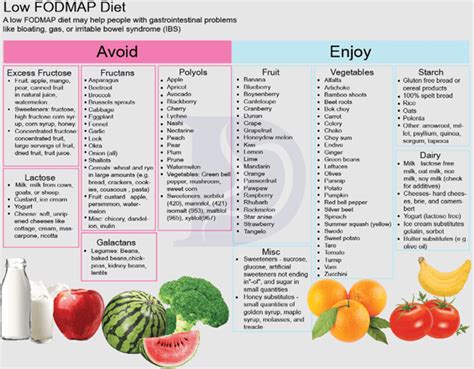
- Diet: Consuming high amounts of sugar, dairy products, and processed foods can feed Candida growth.
- Antibiotics and Medications: Certain medications can disrupt the natural balance of vaginal flora.
- Hygiene and Clothing: Tight clothing, especially when made from non-breathable materials, and poor hygiene practices can create an environment conducive to yeast growth.
- Sexual Activity: While yeast infections are not considered sexually transmitted infections (STIs) in the traditional sense, sexual activity can sometimes trigger or spread an infection.
Cures and Treatments
Fortunately, yeast infections are treatable, and several options are available for managing symptoms and curing the infection:
- Over-the-Counter (OTC) Medications: Antifungal medications like clotrimazole, miconazole, and terconazole are available in various forms, including creams, tablets, and suppositories.
- Prescription Medications: For more severe infections or those that do not respond to OTC treatments, a healthcare provider may prescribe fluconazole (Diflucan), an oral antifungal medication.
- Home Remedies: Natural remedies such as probiotics, tea tree oil, and garlic have been suggested for their antifungal properties, though their effectiveness can vary.
Prevention Strategies
Preventing yeast infections, especially those that seem to recur before periods, involves maintaining good hygiene, wearing breathable clothing, avoiding scented soaps and douching, and practicing safe sex. Dietary changes, including reducing sugar intake and increasing probiotic consumption, may also help. For some women, considering hormonal fluctuations, using gentle, fragrance-free products, and keeping the genital area clean and dry can reduce the risk.
Conclusion
Yeast infections before periods can be a result of the complex interplay between hormonal changes and the body’s natural flora. While these infections can be uncomfortable and frustrating, they are generally treatable with antifungal medications. Prevention strategies, including dietary changes, good hygiene practices, and awareness of contributing factors, can help reduce the risk of recurrence. Understanding the causes and taking proactive steps can empower women to manage their health and comfort throughout their menstrual cycle.
Frequently Asked Questions
How can I tell if I have a yeast infection?
+Common symptoms include itching, redness, and swelling of the vulva, and a thick, white, cottage cheese-like vaginal discharge. If you're experiencing these symptoms, it's essential to consult a healthcare provider for a proper diagnosis and treatment.
Can I prevent yeast infections by using probiotics?
+Probiotics, especially those containing Lactobacillus, can help maintain a healthy balance of vaginal flora and may reduce the risk of yeast infections. However, their effectiveness can vary, and more research is needed to fully understand their benefits in this context.
Why do yeast infections seem to happen before my period?
+The decrease in estrogen levels right before menstruation can affect the vagina's environment, potentially leading to an increased risk of yeast infections. Additionally, changes in the immune system's response and the natural fluctuation in hormonal levels can contribute to this timing.
Understanding and managing yeast infections requires a holistic approach, considering both hormonal and lifestyle factors. By being aware of the causes and taking proactive steps towards prevention and treatment, women can better navigate these issues and maintain their reproductive health throughout their menstrual cycle.