10+ Co 4 Denial Code Solutions To Reduce Claim Rejections
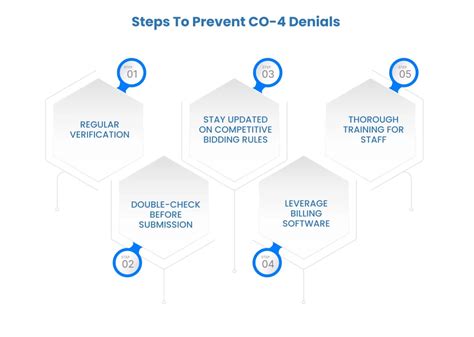
Reducing claim rejections is a critical aspect of managing healthcare revenue cycles effectively. One of the primary challenges healthcare providers face is navigating through the complexities of medical coding and billing, with denial codes playing a significant role in this process. Denial codes, such as those found in the CO (Contractual Obligations) category, provide insight into why a claim has been rejected. CO 4 specifically refers to the denial of a claim due to a lack of information or the submission of incorrect information. Here, we’ll delve into 10+ solutions to address CO 4 denial codes, aiming to reduce claim rejections and streamline the billing process.
1. Enhanced Verification Process
Implementing a rigorous verification process for patient demographics and insurance information can significantly reduce errors that lead to CO 4 denials. This includes validating patient names, dates of birth, policy numbers, and coverage details before submitting claims. Utilizing automated verification tools can improve accuracy and efficiency.
2. Comprehensive Documentation
Maintaining thorough and accurate documentation is crucial. Ensuring that all necessary medical records, including diagnoses, procedures, and treatments, are detailed and up-to-date can help prevent denials due to lack of information. Regular audits can help identify and rectify any gaps in documentation.
3. Coding Accuracy Initiatives
Investing in coding accuracy is paramount. This involves ongoing education and training for coding staff to ensure they are aware of the latest coding updates and guidelines. Implementing coding audits and using coding validation software can also help identify and correct errors before claims are submitted.
4. Improved Communication Channels
Establishing clear and efficient communication channels with patients, providers, and payers can help resolve issues promptly. This includes setting up a system for patients to report changes in their insurance status or demographic information and for providers to query additional information when needed.
5. Automation and Technology Integration
Leveraging technology, such as billing software with built-in editing and verification tools, can automatically check for common errors and inconsistencies in claims before they are submitted. This proactive approach can significantly reduce the likelihood of CO 4 denials.
6. Patient Engagement Strategies
Engaging patients in the process can also yield beneficial outcomes. Educating patients on the importance of their demographic and insurance information accuracy and involving them in the verification process can help ensure that all necessary information is correct and up-to-date.
7. Regular Payer Updates
Payer policies and requirements can change frequently. Regularly updating payer information and ensuring that billing staff are aware of these changes can prevent denials due to non-compliance with payer-specific requirements.
8. Denial Analysis and Trending
Conducting regular analysis of denial trends can help identify systemic issues that may be contributing to CO 4 denials. By understanding the root causes, targeted interventions can be developed to address these issues proactively.
9. Staff Training and Education
Providing ongoing training and education to billing and coding staff is essential. This should include training on the latest coding guidelines, payer policies, and billing software to ensure that staff have the knowledge and skills needed to accurately and efficiently process claims.
10. Quality Assurance Programs
Implementing quality assurance programs can help ensure that claims are thoroughly reviewed for accuracy and completeness before submission. This can include pre-bill audits and regular review of denied claims to identify areas for improvement.
11. Adoption of Advanced Data Analytics
Utilizing advanced data analytics can provide insights into claim submission patterns, denial rates, and areas where processes can be improved. This data-driven approach can help in developing targeted strategies to reduce CO 4 denials.
Conclusion
Addressing CO 4 denial codes requires a multifaceted approach that encompasses enhanced verification processes, comprehensive documentation, coding accuracy initiatives, and the adoption of technology and data analytics. By implementing these solutions and continually assessing and improving billing and coding practices, healthcare providers can significantly reduce claim rejections and improve the efficiency of their revenue cycle management.
FAQs
What is a CO 4 denial code, and how does it affect claim processing?
+A CO 4 denial code indicates that a claim has been rejected due to a lack of information or the submission of incorrect information. This can significantly delay the claim processing timeline and impact revenue cycles if not addressed promptly.
How can healthcare providers reduce CO 4 denial codes?
+Healthcare providers can reduce CO 4 denial codes by implementing rigorous verification processes, ensuring comprehensive documentation, investing in coding accuracy, and leveraging technology and data analytics to identify and rectify errors before claim submission.
What role does patient engagement play in reducing CO 4 denial codes?
+Patient engagement is crucial as it involves patients in the verification process of their demographic and insurance information, helping to ensure accuracy and completeness of the information provided, which in turn can reduce CO 4 denials.
By focusing on these strategies, healthcare providers can not only reduce CO 4 denial codes but also enhance the overall efficiency and effectiveness of their billing and revenue cycle management processes.