10+ Ekg Secrets For Accurate Results

The electrocardiogram (EKG or ECG) is a fundamental diagnostic tool in cardiology, providing crucial information about the heart’s electrical activity. However, to ensure accurate results, it’s essential to be aware of several secrets that can significantly impact the quality and interpretation of EKG readings. In this comprehensive guide, we’ll delve into over 10 EKG secrets that every healthcare professional should know to enhance their diagnostic skills and provide better patient care.
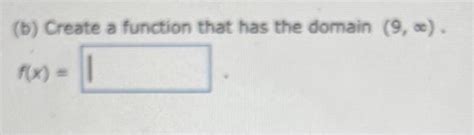
1. Standardization is Key
Ensuring that the EKG machine is properly calibrated and that the electrodes are placed correctly according to standard guidelines (such as the Mason-Likar system for exercise testing or the standard 12-lead placement for diagnostic EKGs) is crucial. Incorrect placement can lead to misleading results, including misinterpretation of arrhythmias or ischemia.
2. Skin Preparation Matters
Before applying electrodes, the skin should be properly prepared. This includes cleaning the area with alcohol to remove oils and lotions, shaving if necessary, and slightly abrading the skin to improve electrode contact. Good skin-electrode contact is vital for clear signal acquisition.
3. Reduction of Electrical Interference
Electrical interference from external sources (such as fluorescent lights, nearby electrical equipment, or even the patient’s own muscular activity) can significantly degrade the quality of the EKG tracing. Strategies to minimize interference include using shielded cables, placing the EKG machine in a quiet area, and ensuring the patient remains as still as possible during the recording.
4. Patient Positioning Can Affect Results
The position of the patient can influence the EKG tracing. For example, the right arm should be relaxed and not compressed against the body, as this can alter the electrical axis. Similarly, deep breathing can affect some EKG parameters. Awareness of these factors can help in obtaining more accurate and reproducible results.
5. Lead Selection for Specific Diagnoses
Different leads provide different views of the heart, making some more suitable than others for diagnosing specific conditions. For instance, leads II, III, and aVF are particularly useful for detecting inferior wall ischemia, while leads V1 and V2 are more informative for anterior wall ischemia.
6. Understanding Artifacts
Artifacts are distortions in the EKG tracing not related to the heart’s electrical activity. They can be caused by muscle movement, electrical interference, or issues with the electrodes or machine. Recognizing these artifacts is crucial to avoid misinterpreting them as pathological findings.
7. The Role of Filter Settings
Modern EKG machines often come with filter settings designed to reduce certain types of interference. However, these filters can also potentially remove or distort important clinical information. Understanding when and how to apply these filters can significantly impact the diagnostic utility of the EKG.
8. Monitoring vs. Diagnostic EKG
While diagnostic EKGs provide a snapshot of the heart’s electrical activity at a single point in time, monitoring (such as with Holter or event monitors) can capture transient events that might not be evident on a standard EKG. Knowing when to use each can be critical in detecting intermittent arrhythmias or ischemic episodes.
9. The Importance of Baseline Measurements
Establishing baseline measurements for each patient is vital. This allows for the detection of changes over time, which can be critical in monitoring the progression of disease or the effectiveness of treatment.
10. Continuous Learning
EKG interpretation is a skill that requires continuous learning and practice. Staying updated with the latest guidelines, attending workshops, and regularly reviewing EKG tracings can enhance one’s skills in identifying subtle abnormalities and accurately interpreting EKG results.
11. Integrating Clinical Context
Interpreting an EKG in isolation can lead to errors. Incorporating the patient’s clinical history, physical examination findings, and results from other diagnostic tests into the interpretation can significantly enhance the accuracy of EKG readings.
12. Utilizing EKG in Different Populations
EKG patterns can vary between different age groups and in specific conditions. For example, the pediatric EKG has distinct features compared to the adult EKG, and certain conditions like Wolff-Parkinson-White syndrome have characteristic EKG findings. Being aware of these variations is essential for accurate interpretation.
13. Digital vs. Analog Interpretation
With the advent of digital EKG systems, the ease and speed of accessing and interpreting EKGs have improved. However, the transition from analog to digital also introduces new challenges, such as ensuring the fidelity of digital recordings and being aware of the limitations of digital measurement tools.
Conclusion
The EKG is a powerful tool in the diagnosis and management of cardiac conditions, but its utility is highly dependent on the quality of the recording and the skill of the interpreter. By mastering the secrets outlined above, healthcare professionals can significantly enhance their ability to obtain accurate and clinically useful information from EKGs, ultimately leading to better patient outcomes.
What is the most common cause of inaccurate EKG results?
+One of the most common causes of inaccurate EKG results is improper electrode placement. Ensuring that electrodes are placed according to standard guidelines can significantly reduce errors in EKG interpretation.
How can electrical interference be minimized during an EKG?
+Electrical interference can be minimized by using shielded cables, placing the EKG machine in a quiet area away from other electrical equipment, and ensuring the patient remains as still as possible during the recording. Additionally, proper skin preparation and electrode placement can help reduce noise.
What is the significance of continuous learning in EKG interpretation?
+Continuous learning is crucial in EKG interpretation as it helps healthcare professionals stay updated with the latest guidelines, enhance their skills in identifying subtle abnormalities, and accurately interpret EKG results in the context of evolving medical knowledge and technology.