12 Co 4 Denial Code Fixes For Faster Approval
The frustration of dealing with insurance claims and denials is a common experience for many healthcare providers and patients alike. One of the most critical aspects of navigating this complex system is understanding and effectively addressing denial codes. In this comprehensive guide, we will delve into the world of denial code fixes, focusing on 12 CO and 4 DEN codes that are crucial for faster approval and reimbursement.
Understanding Denial Codes
Before we dive into the specifics of 12 CO and 4 DEN codes, it’s essential to understand what denial codes are and their role in the insurance claims process. Denial codes are numerical codes used by insurance companies to communicate the reason for denying a claim. These codes are part of the Claim Adjustment Reason Codes set, which standardizes the reasons for claim denials across the industry.
12 CO Denial Code
The 12 CO denial code is used to indicate that the service was not authorized or the treatment plan was not approved. This denial can often be resolved by obtaining the necessary authorization or approval from the insurance company before providing the service. Here are some steps you can take to address a 12 CO denial:
- Verify Patient Eligibility: Ensure that the patient has active coverage with the insurance company.
- Obtain Pre-Authorization: For certain treatments or services, pre-authorization from the insurance company is required. Submit the required documentation to obtain approval.
- Submit Correct Claims: Ensure that all claims submitted are accurate and complete, with the correct billing and diagnosis codes.
- Appeal the Denial: If you believe the denial was incorrect, you can appeal the decision by providing additional information or clarification.
4 DEN Denial Code
The 4 DEN denial code signifies that the procedure code is inconsistent with the patient’s condition or the provider’s depiction of the service. This denial highlights the importance of accurate coding in the billing process. Here are some strategies to address a 4 DEN denial:
- Review Coding Accuracy: Ensure that the procedure codes and diagnosis codes used are correct and appropriate for the service provided.
- Clinical Documentation: Verify that the clinical documentation supports the codes used for billing. This includes ensuring that the documentation clearly explains the medical necessity of the service.
- Coding Updates: Stay updated with the latest coding guidelines and changes. Regular training for coding staff can help in minimizing coding errors.
- Coding Consistency: Implement a system to ensure coding consistency across the organization to reduce the likelihood of inconsistent coding practices.
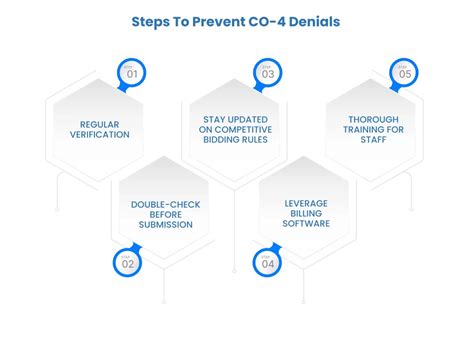
Strategies for Faster Approval
Faster approval of insurance claims requires a proactive approach to addressing denial codes and improving the overall claims submission process. Here are several strategies you can implement:
- Automate Claims Submission: Utilize electronic claims submission to reduce errors and increase the speed of the process.
- Pre-Claim Review: Conduct a thorough review of claims before submission to identify and correct potential issues.
- Regular Follow-Up: Establish a follow-up process for submitted claims to ensure they are being processed and address any issues promptly.
- Provider Education: Educate healthcare providers on the importance of complete and accurate documentation, as well as the latest coding guidelines.
- Patient Engagement: Engage patients in the process by informing them about the need for pre-authorizations and the importance of providing accurate demographic and insurance information.
Conclusion
Addressing denial codes such as 12 CO and 4 DEN requires a comprehensive understanding of the insurance claims process and a proactive approach to resolving issues. By implementing strategies for accurate coding, obtaining necessary pre-authorizations, and ensuring complete documentation, healthcare providers can significantly reduce denials and achieve faster approval of their claims. Continuous education and training in coding and billing practices, along with leveraging technology for efficient claims processing, are key to navigating the complex landscape of insurance claims and denials.
What are denial codes, and why are they used in insurance claims?
+Denial codes are numerical codes used by insurance companies to communicate the reason for denying a claim. They are part of the Claim Adjustment Reason Codes set and play a crucial role in standardizing the reasons for claim denials across the industry.
How can I address a 12 CO denial code for lack of pre-authorization?
+To address a 12 CO denial, verify the patient’s eligibility, obtain pre-authorization for the service, ensure accurate claims submission, and consider appealing the denial if necessary.
What steps can be taken to reduce 4 DEN denial codes related to inconsistent procedure codes?
+Reducing 4 DEN denial codes involves reviewing coding accuracy, ensuring clinical documentation supports the codes used, staying updated with coding guidelines, and implementing a system for coding consistency.