Abo And Rh
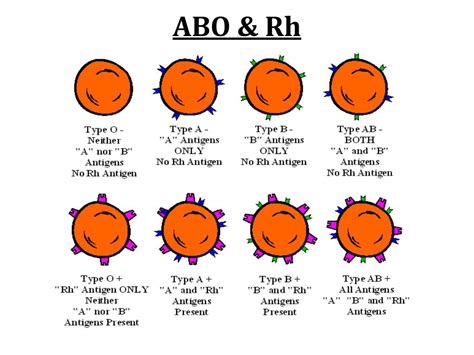
The ABO and Rh blood group systems are two of the most important blood types in transfusion medicine. Understanding these systems is crucial for ensuring safe blood transfusions and preventing adverse reactions.
The ABO blood group system was discovered in 1901 by Austrian physician Karl Landsteiner, who identified the A and B antigens on red blood cells. Later, in 1911, Landsteiner and Alfred von Decastello discovered the AB blood group, and in 1940, Alexander S. Wiener and Karl Landsteiner discovered the Rh blood group system.
ABO Blood Group System
The ABO blood group system is based on the presence or absence of specific antigens on the surface of red blood cells. There are four main ABO blood types:
- Type A: Red blood cells have A antigens on their surface.
- Type B: Red blood cells have B antigens on their surface.
- Type AB: Red blood cells have both A and B antigens on their surface.
- Type O: Red blood cells have neither A nor B antigens on their surface.
Individuals with Type A blood can receive blood from Type A or Type O donors, while those with Type B blood can receive from Type B or Type O donors. People with Type AB blood are often referred to as “universal recipients” because they can receive blood from all four ABO blood types (A, B, AB, and O). Conversely, those with Type O blood are known as “universal donors” since their blood can be transfused to individuals with any ABO blood type.
Rh Blood Group System
The Rh blood group system is another critical blood type classification. It is based on the presence or absence of the RhD antigen on red blood cells. There are two main Rh blood types:
- Rh-positive: Red blood cells have the RhD antigen on their surface.
- Rh-negative: Red blood cells do not have the RhD antigen on their surface.
It is crucial for pregnant women to know their Rh blood type, as an incompatibility between the mother’s and fetus’s Rh types can lead to complications. If an Rh-negative mother is pregnant with an Rh-positive fetus, the mother’s immune system may react to the Rh-positive blood cells of the fetus. This reaction can cause the production of antibodies against the RhD antigen, which may lead to hemolysis (breakdown of red blood cells) in the fetus.
Clinical Significance and Implications
Understanding the ABO and Rh blood group systems is essential for several clinical applications:
- Blood Transfusions: Knowing a patient’s ABO and Rh blood types is critical for selecting compatible blood products for transfusions, minimizing the risk of adverse reactions.
- Pregnancy and Childbirth: Determining the Rh blood type of pregnant women and their partners helps identify potential risks and guides appropriate management to prevent complications.
- Organ Transplantation: ABO and Rh blood type compatibility is crucial for matching organ donors and recipients, reducing the risk of rejection and graft failure.
In conclusion, the ABO and Rh blood group systems play a vital role in transfusion medicine, pregnancy, and organ transplantation. Proper identification and understanding of these blood types are critical for ensuring safe medical practices and preventing adverse reactions.
What is the difference between ABO and Rh blood group systems?
+The ABO blood group system is based on the presence or absence of A and B antigens on red blood cells, while the Rh blood group system is based on the presence or absence of the RhD antigen.
Why is it important to know one’s ABO and Rh blood types?
+Knowing one’s ABO and Rh blood types is essential for ensuring safe blood transfusions, preventing complications during pregnancy and childbirth, and matching organ donors and recipients for transplantation.
Can individuals with different ABO blood types donate blood to each other?
+No, individuals with different ABO blood types should not donate blood to each other, as this can lead to severe adverse reactions. However, individuals with Type O blood can donate to those with any ABO blood type, and those with Type AB blood can receive from any ABO blood type.