Amox/K Clav 875125: Effective Bacterial Infection Treatment
Bacterial infections pose a significant threat to human health, with the potential to cause severe symptoms and even life-threatening complications if left untreated. The rise of antibiotic-resistant bacteria has further complicated the treatment landscape, necessitating the use of potent and targeted therapeutic agents. Among the arsenal of antibiotics available, Amox/K Clav 875⁄125, a combination of amoxicillin and clavulanic acid, has emerged as a highly effective treatment option for a wide range of bacterial infections.
Understanding Amox/K Clav 875⁄125

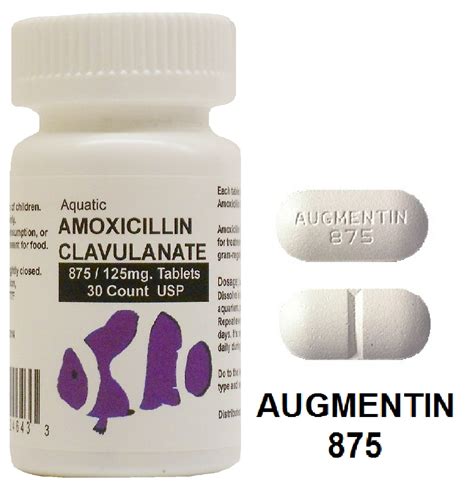
Amox/K Clav 875⁄125 is an oral antibiotic that combines the broad-spectrum penicillin antibiotic amoxicillin with clavulanic acid, a beta-lactamase inhibitor. This synergistic combination enhances the efficacy of amoxicillin by protecting it from degradation by beta-lactamase enzymes, which are produced by certain bacteria. This mechanism allows Amox/K Clav 875⁄125 to maintain its antibacterial potency against a broader spectrum of pathogens, including many strains that are resistant to other antibiotics.
Mechanism of Action
The therapeutic effect of Amox/K Clav 875⁄125 is rooted in its ability to inhibit bacterial cell wall synthesis. Amoxicillin interferes with the formation of the bacterial cell wall by binding to penicillin-binding proteins (PBPs), which are essential for the cross-linking of peptidoglycan layers. Without a functional cell wall, bacterial cells cannot maintain their structural integrity, leading to cell lysis and death. Clavulanic acid extends the antimicrobial spectrum of amoxicillin by inactivating beta-lactamase enzymes, thereby preventing the degradation of amoxicillin and ensuring its continued bactericidal activity.
Clinical Applications

Amox/K Clav 875⁄125 is indicated for the treatment of various bacterial infections, including:
- Acute Bacterial Sinusitis: Infections of the paranasal sinuses, which can cause symptoms such as facial pain, nasal congestion, and purulent discharge.
- Community-Acquired Pneumonia: A serious infection of the lungs that can be caused by a variety of bacteria, including Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
- Skin and Soft Tissue Infections: Includes conditions like cellulitis, where the skin and underlying tissues become infected, and abscesses, which are localized collections of pus.
- Urinary Tract Infections: Infections of the kidneys, bladder, or urethra, which can cause dysuria, frequent urination, and abdominal pain.
- Bite Wounds: Human or animal bites can introduce bacteria into the wound, leading to infection. Amox/K Clav 875⁄125 is effective against many of the pathogens commonly found in such wounds.
Dosage and Administration
The dosage of Amox/K Clav 875⁄125 is typically determined by the severity and location of the infection, as well as patient factors such as age, weight, and renal function. The standard adult dosage for most infections is 875 mg of amoxicillin and 125 mg of clavulanic acid, administered orally every 12 hours or 500 mg of amoxicillin and 125 mg of clavulanic acid every 8 hours. It is crucial to complete the full treatment course as directed by a healthcare provider, even if symptoms improve before finishing the medication, to ensure the eradication of the infection and prevent the development of antibiotic resistance.
Side Effects and Precautions
While Amox/K Clav 875⁄125 is generally well-tolerated, it can cause side effects, including:
- Gastrointestinal Upset: Nausea, vomiting, and diarrhea are common side effects.
- Rash: Some patients may develop a skin rash.
- Hypersensitivity Reactions: Rare but serious allergic reactions can occur, including anaphylaxis and Stevens-Johnson syndrome.
It is essential to monitor for signs of allergic reactions, especially in patients with a history of penicillin allergy. Additionally, Amox/K Clav 875⁄125 can interact with other medications, such as anticoagulants and oral contraceptives, necessitating careful consideration of potential drug interactions.
Resistance and Stewardship
The increasing prevalence of antibiotic-resistant bacteria underscores the importance of judicious antibiotic use. The misuse and overuse of antibiotics, including Amox/K Clav 875⁄125, can accelerate the development of resistance. Healthcare providers must adhere to principles of antibiotic stewardship, prescribing antibiotics only when necessary and selecting the most appropriate agent based on the suspected or confirmed causative pathogen, local resistance patterns, and patient-specific factors.
Conclusion
Amox/K Clav 875⁄125 represents a powerful tool in the treatment of bacterial infections, offering a broad spectrum of activity against a wide range of pathogens. Its effectiveness, combined with its relatively favorable safety profile, makes it a valuable option in the management of various infections. However, its use must be tempered by the principles of antibiotic stewardship to preserve its efficacy for future generations. As the landscape of bacterial infections continues to evolve, the strategic use of Amox/K Clav 875⁄125, alongside other antibiotics and adjunctive therapies, will remain crucial in the fight against bacterial diseases.
What is the primary mechanism of action of Amox/K Clav 875⁄125?
+The primary mechanism of action involves the inhibition of bacterial cell wall synthesis by amoxicillin, which is protected from degradation by beta-lactamase enzymes through the action of clavulanic acid.
For which types of infections is Amox/K Clav 875⁄125 typically prescribed?
+Amox/K Clav 875⁄125 is prescribed for a variety of bacterial infections, including acute bacterial sinusitis, community-acquired pneumonia, skin and soft tissue infections, urinary tract infections, and bite wounds.
What precautions should be taken to avoid the development of antibiotic resistance?
+To avoid the development of antibiotic resistance, antibiotics like Amox/K Clav 875⁄125 should only be used when necessary, and the full treatment course should be completed as directed. Additionally, healthcare providers should follow principles of antibiotic stewardship, selecting the most appropriate antibiotic based on the suspected causative pathogen and local resistance patterns.