Bleeding After Sex

Bleeding after sexual intercourse, also known as postcoital bleeding, is a symptom that can cause concern and anxiety for many individuals. It’s essential to understand the potential causes, risk factors, and when to seek medical attention. Bleeding after sex can occur in people of all ages, but it’s more common in women, particularly those of reproductive age.
Causes of Bleeding After Sex
There are several possible causes of bleeding after sex, ranging from harmless to more serious conditions. Some of the most common causes include:
- Cervical Erosion: A condition where the cervix becomes inflamed, causing bleeding. This can be due to a variety of factors, including hormonal changes, infection, or physical trauma.
- Cervical Polyps: Small, non-cancerous growths on the cervix that can bleed after sex.
- Endometrial Atrophy: Thinning of the uterine lining, which can cause bleeding, especially in postmenopausal women.
- Vaginal Dryness: Insufficient lubrication during sex can cause friction, leading to bleeding.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs that can cause bleeding, pain, and other symptoms.
- Cancer: Although rare, cervical, uterine, or ovarian cancer can cause bleeding after sex.
- Hormonal Changes: Fluctuations in hormone levels, such as those experienced during menopause or with certain birth control methods, can lead to bleeding.
- Trauma: Physical trauma to the vagina, cervix, or uterus during sex can cause bleeding.
Risk Factors
Certain factors can increase the risk of bleeding after sex, including:
- Age: Women over 40 are more likely to experience bleeding after sex due to hormonal changes and age-related wear and tear on the reproductive organs.
- Menopause: The decline in estrogen levels during menopause can lead to vaginal dryness and bleeding.
- Sexually Transmitted Infections (STIs): Certain STIs, such as chlamydia or gonorrhea, can cause bleeding and other symptoms.
- Previous Gynecological Conditions: Women with a history of gynecological conditions, such as cervical dysplasia or endometriosis, may be more likely to experience bleeding after sex.
- Sexual Practices: Rough sex, multiple partners, or certain sex toys can increase the risk of bleeding.
When to Seek Medical Attention
While occasional bleeding after sex may not be a cause for concern, it’s essential to seek medical attention if:
- Bleeding is Heavy or Prolonged: If bleeding is heavy, lasts for more than a few days, or soaks through more than one pad or tampon per hour.
- Pain is Severe: If pain is severe, persistent, or accompanied by other symptoms like fever, chills, or vaginal discharge.
- Bleeding is Accompanied by Other Symptoms: If bleeding is accompanied by other symptoms like abdominal pain, nausea, or vomiting.
- You’re Experiencing Unusual Discharge: If you notice unusual discharge, odor, or color, which can be a sign of an infection.
- You’re Concerned or Anxious: If you’re concerned or anxious about bleeding after sex, it’s always best to consult with a healthcare provider for reassurance and guidance.
Diagnosis and Treatment
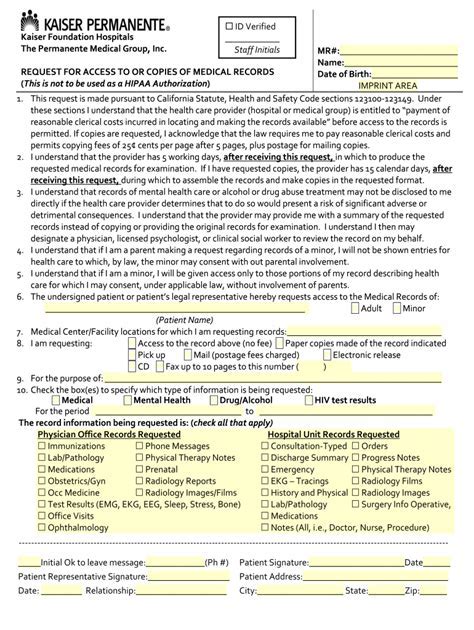
If you experience bleeding after sex, your healthcare provider will likely perform a physical exam, take a medical history, and may recommend additional tests, such as:
- Pelvic Exam: A thorough exam of the reproductive organs to check for any abnormalities or signs of infection.
- Pap Test: A test to check for abnormal cell changes on the cervix.
- Ultrasound: An imaging test to evaluate the uterus, ovaries, and other reproductive organs.
- Blood Tests: To check for underlying conditions, such as anemia or infection.
Treatment will depend on the underlying cause of bleeding, but may include:
- Hormonal Therapy: To regulate hormonal imbalances or treat conditions like endometrial atrophy.
- Antibiotics: To treat infections, such as PID or STIs.
- Pain Management: To alleviate pain and discomfort.
- Surgery: In some cases, surgery may be necessary to remove cervical polyps, treat cancer, or repair any damage to the reproductive organs.
Prevention and Management
While some cases of bleeding after sex may be unavoidable, there are steps you can take to reduce the risk:
- Practice Safe Sex: Use condoms or other barrier methods to reduce the risk of STIs and unwanted pregnancy.
- Use Lubrication: Apply lubrication during sex to reduce friction and prevent vaginal dryness.
- Maintain Good Hygiene: Keep the genital area clean and dry to prevent infections.
- Get Regular Check-Ups: Schedule regular gynecological exams to monitor your reproductive health and catch any potential issues early.
What are the most common causes of bleeding after sex?
+The most common causes of bleeding after sex include cervical erosion, cervical polyps, endometrial atrophy, vaginal dryness, and pelvic inflammatory disease (PID).
When should I seek medical attention for bleeding after sex?
+Seek medical attention if bleeding is heavy or prolonged, accompanied by severe pain, or if you're experiencing unusual discharge or other symptoms.
How can I reduce the risk of bleeding after sex?
+Practice safe sex, use lubrication, maintain good hygiene, and get regular check-ups to reduce the risk of bleeding after sex.
In conclusion, bleeding after sex can be a concerning symptom, but it’s essential to understand the potential causes, risk factors, and when to seek medical attention. By taking proactive steps to maintain good reproductive health and seeking medical attention when necessary, you can reduce the risk of bleeding after sex and ensure your overall well-being.