Blood Thinner Medications
Blood thinner medications, also known as anticoagulants, are a crucial part of managing and preventing blood clots, which can lead to serious health conditions such as stroke, heart attack, and pulmonary embolism. These medications work by slowing down the formation of blood clots or preventing existing clots from growing. In this comprehensive guide, we will delve into the world of blood thinner medications, exploring their types, mechanisms, benefits, and risks, as well as providing expert insights and practical advice for individuals taking these medications.
Understanding Blood Clots and Anticoagulation
To appreciate the importance of blood thinner medications, it’s essential to understand how blood clots form and the role of anticoagulation in preventing them. Blood clots are complex structures composed of platelets, fibrin, and other blood cells that aggregate in response to injury or inflammation. While blood clots are a natural response to bleeding, they can become a problem when they form inappropriately, such as in deep veins or arteries, leading to potentially life-threatening conditions.
Anticoagulation, the process of preventing blood clot formation or growth, is critical in managing conditions like atrial fibrillation, deep vein thrombosis (DVT), and pulmonary embolism. Blood thinner medications achieve this by targeting various points in the coagulation cascade, a complex series of reactions that lead to blood clot formation.
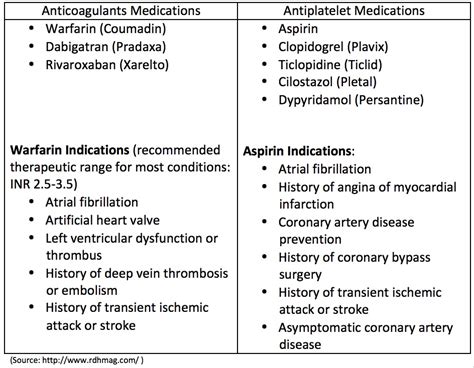
Types of Blood Thinner Medications
There are several types of blood thinner medications, each with its unique mechanism of action, benefits, and risks. The most common categories include:
- Warfarin (Coumadin): A vitamin K antagonist that works by inhibiting the production of vitamin K-dependent clotting factors. Warfarin is one of the oldest and most widely used anticoagulants, but it requires regular monitoring of international normalized ratio (INR) levels to ensure therapeutic efficacy and minimize bleeding risks.
- Direct Oral Anticoagulants (DOACs): A class of medications that directly inhibit specific clotting factors, such as factor IIa (thrombin) or factor Xa. DOACs, including apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa), offer a more predictable pharmacokinetic profile and reduced monitoring requirements compared to warfarin.
- Heparin: A fast-acting anticoagulant that works by activating antithrombin, a natural anticoagulant protein. Heparin is often used in acute settings, such as during hospitalization for DVT or pulmonary embolism, and can be administered intravenously or subcutaneously.
- Aspirin: An antiplatelet agent that works by inhibiting platelet aggregation, thereby reducing the risk of blood clot formation. Aspirin is commonly used in low doses to prevent cardiovascular events, such as heart attack and stroke.
Benefits and Risks of Blood Thinner Medications
While blood thinner medications are essential for managing and preventing blood clots, they also carry potential benefits and risks. The benefits include:
- Reduced risk of blood clots and related complications, such as stroke and heart attack
- Improved quality of life for individuals with conditions like atrial fibrillation or DVT
- Prevention of recurrent blood clots in individuals with a history of clotting disorders
However, the risks associated with blood thinner medications include:
- Bleeding complications, ranging from minor bruising to life-threatening hemorrhage
- Interactions with other medications, such as antibiotics or anti-inflammatory agents
- Increased risk of bleeding with traumatic injury or surgical procedures
- Potential for adverse effects, such as skin rash or liver dysfunction, with certain medications
Expert Insights and Practical Advice
For individuals taking blood thinner medications, it’s essential to balance the benefits of anticoagulation with the risks of bleeding and other complications. Here are some expert insights and practical tips:
- Regular monitoring: Regular monitoring of INR levels (for warfarin) or renal function (for DOACs) is crucial to ensure therapeutic efficacy and minimize bleeding risks.
- Medication adherence: Adhering to the prescribed medication regimen and dosage is vital to maintain optimal anticoagulation and reduce the risk of bleeding complications.
- Lifestyle modifications: Making lifestyle modifications, such as avoiding excessive alcohol consumption, quitting smoking, and maintaining a healthy weight, can help reduce the risk of bleeding complications and improve overall health.
- Communication with healthcare providers: Open communication with healthcare providers is essential to discuss concerns, report any changes in medication or health status, and address potential interactions with other medications.
FAQ Section
What are the most common side effects of blood thinner medications?
+The most common side effects of blood thinner medications include bleeding complications, such as bruising, nosebleeds, or gastrointestinal bleeding. Other potential side effects may include skin rash, liver dysfunction, or increased risk of infection.
Can I take blood thinner medications with other medications, such as antibiotics or pain relievers?
+It's essential to consult with your healthcare provider before taking any new medications, including antibiotics or pain relievers, while on blood thinner medications. Certain medications may interact with anticoagulants, increasing the risk of bleeding complications or reducing their effectiveness.
How long do I need to take blood thinner medications?
+The duration of blood thinner medication therapy depends on the underlying condition, individual risk factors, and response to treatment. Your healthcare provider will determine the optimal treatment duration and monitor your condition regularly to adjust the treatment plan as needed.
In conclusion, blood thinner medications are a vital component of managing and preventing blood clots, and their benefits and risks must be carefully considered. By understanding the different types of anticoagulants, their mechanisms, and potential complications, individuals can make informed decisions about their treatment and work closely with healthcare providers to minimize risks and maximize benefits. Remember, blood thinner medications are a powerful tool in preventing life-threatening conditions, and with careful management and adherence to treatment plans, individuals can reduce their risk of blood clots and improve their overall quality of life.