Losartan Uses Revealed: Blood Pressure Control

Losartan, a medication belonging to the class of angiotensin II receptor antagonists (ARBs), has been a cornerstone in the management of hypertension and heart failure for decades. Its mechanism of action, which involves blocking the angiotensin II type 1 receptor, leads to vasodilation and a subsequent reduction in blood pressure. This article delves into the multifaceted uses of losartan, its efficacy in controlling blood pressure, and its role in managing other cardiovascular conditions, highlighting its importance in modern cardiology.
Historical Evolution of Losartan
The development of losartan marked a significant milestone in the treatment of hypertension. Introduced in the 1990s, it was the first angiotensin II receptor antagonist to be approved for clinical use. Since then, losartan has undergone extensive research, and its applications have expanded beyond hypertension to include the treatment of diabetic nephropathy and heart failure. Understanding the historical context of losartan’s development provides insight into its pharmacological properties and therapeutic applications.
Pharmacological Profile
Losartan’s pharmacological profile is characterized by its high affinity for the angiotensin II type 1 receptor. By competitively inhibiting the binding of angiotensin II to its receptor, losartan prevents vasoconstriction and reduces aldosterone secretion, leading to decreased peripheral resistance and lowered blood pressure. Additionally, losartan has a unique active metabolite, E-3174, which contributes significantly to its therapeutic effects. This dual mechanism of action distinguishes losartan from other antihypertensive agents and underscores its efficacy in managing hypertension.
Clinical Applications
Hypertension Management
The primary indication for losartan is the treatment of essential hypertension. Clinical trials have consistently demonstrated losartan’s ability to lower blood pressure effectively in patients with mild to moderate hypertension. Its use is particularly recommended for patients who cannot tolerate ACE inhibitors due to side effects such as cough. Losartan’s safety profile, combined with its efficacy, makes it a preferred choice for long-term blood pressure management.
Diabetic Nephropathy
Beyond its antihypertensive effects, losartan has been shown to slow the progression of diabetic nephropathy, a leading cause of end-stage renal disease in patients with type 2 diabetes. By reducing proteinuria and minimizing the decline in glomerular filtration rate, losartan plays a crucial role in preserving renal function. The RENAAL study, among others, has provided robust evidence supporting the renoprotective effects of losartan in diabetic patients.
Heart Failure
Losartan is also used in the treatment of heart failure, particularly in patients who are intolerant to ACE inhibitors. It helps to reduce morbidity and mortality by counteracting the harmful effects of angiotensin II on the heart and blood vessels. While the evidence for its use in heart failure is not as extensive as for hypertension, losartan remains a valuable option for managing this condition, especially when used in combination with other heart failure therapies.
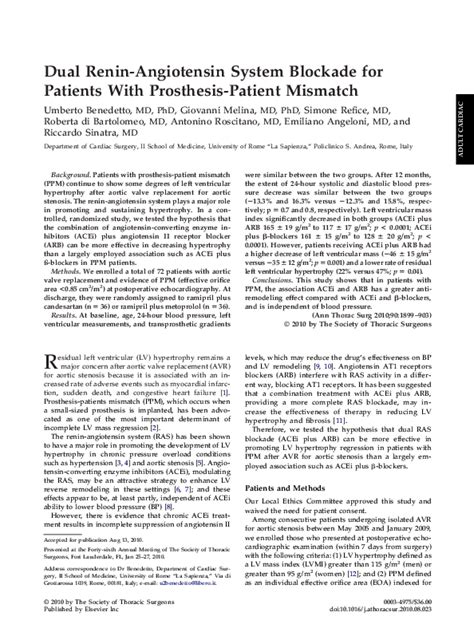
Comparative Analysis with Other Antihypertensive Agents
When comparing losartan with other classes of antihypertensive drugs, such as calcium channel blockers, beta-blockers, and diuretics, it’s clear that each has its unique advantages and disadvantages. Losartan’s ability to offer renal protection and its favorable side effect profile make it an attractive option for many patients. However, the choice of antihypertensive therapy should be individualized, considering factors such as the patient’s comorbidities, potential drug interactions, and lifestyle.
Practical Application Guide
For healthcare providers considering losartan for their patients, several key points are worth noting: - Dosage and Titration: Losartan can be initiated at a dose of 50 mg once daily, with titration to 100 mg daily if necessary, based on blood pressure response. - Monitoring: Regular monitoring of blood pressure, renal function, and electrolyte levels is essential during losartan therapy. - Combination Therapy: Losartan can be used in combination with other antihypertensive agents, including diuretics, calcium channel blockers, and beta-blockers, to achieve better blood pressure control.
Scenario-Based Examples
Consider a 55-year-old diabetic patient with hypertension and mild renal impairment. Losartan would be an excellent choice for this patient due to its ability to control blood pressure while offering renoprotective effects. In contrast, for a patient with heart failure and a history of ACE inhibitor-induced cough, losartan could serve as a suitable alternative to manage both heart failure and hypertension.
Decision Framework forChoosing Losartan
When deciding whether losartan is the appropriate antihypertensive agent for a patient, consider the following criteria: 1. Presence of Diabetic Nephropathy: Losartan’s renoprotective effects make it an ideal choice for patients with diabetic nephropathy. 2. Intolerance to ACE Inhibitors: For patients who cannot tolerate ACE inhibitors due to side effects, losartan is a viable alternative. 3. Heart Failure: Losartan can be used in the management of heart failure, especially in patients intolerant to ACE inhibitors.
Myth vs. Reality: common misconceptions about losartan
- Myth: Losartan is less effective than ACE inhibitors in reducing blood pressure.
- Reality: Losartan is as effective as ACE inhibitors in lowering blood pressure and offers additional benefits such as renal protection.
- Myth: Losartan is not suitable for patients with heart failure.
- Reality: Losartan can be used in the treatment of heart failure, particularly in patients who are intolerant to ACE inhibitors.
Future Trends Projection
As research continues to uncover the complex mechanisms underlying cardiovascular diseases, the role of losartan and other ARBs is likely to evolve. Emerging evidence suggests that these drugs may have protective effects beyond blood pressure reduction, including anti-inflammatory and antioxidant properties. Future studies will be crucial in fully elucidating these effects and exploring new therapeutic applications for losartan.
Conclusion
Losartan’s versatility as an antihypertensive agent, coupled with its protective effects on the kidneys and potential benefits in heart failure, solidifies its position as a cornerstone in cardiovascular therapy. By understanding its pharmacological profile, clinical applications, and practical considerations for use, healthcare providers can maximize the benefits of losartan for their patients, contributing to improved cardiovascular health outcomes.
What is the primary mechanism of action of losartan?
+Losartan works by blocking the angiotensin II type 1 receptor, leading to vasodilation and a reduction in blood pressure.
Can losartan be used in patients with diabetic nephropathy?
+Yes, losartan has been shown to slow the progression of diabetic nephropathy and is recommended for patients with type 2 diabetes.
Is losartan suitable for patients with heart failure?
+Losartan can be used in the treatment of heart failure, particularly in patients who are intolerant to ACE inhibitors.
| Medication | Primary Use | Unique Benefits |
|---|---|---|
| Losartan | Hypertension, Diabetic Nephropathy, Heart Failure | Renoprotective effects, suitable for patients intolerant to ACE inhibitors |
| ACE Inhibitors | Hypertension, Heart Failure, Diabetic Nephropathy | Proven to reduce morbidity and mortality in heart failure and diabetic nephropathy |
| Calcium Channel Blockers | Hypertension | Particularly effective in older patients and those with certain types of hypertension |