Co 4 Denial Code

The CO 4 Denial Code, also known as the “Denial Code CO 4,” is a term commonly used in the context of medical billing and insurance claims. In this article, we will delve into the specifics of the CO 4 Denial Code, exploring its definition, causes, and implications for healthcare providers and patients alike. Our goal is to provide a comprehensive understanding of this denial code, including strategies for appeal and prevention.
Introduction to the CO 4 Denial Code
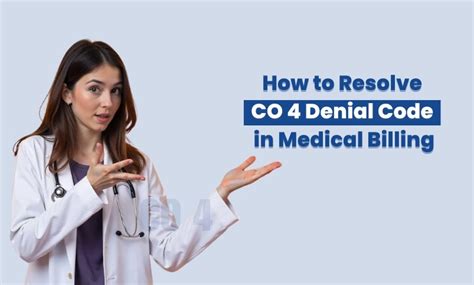
The CO 4 Denial Code is utilized by insurance companies to indicate that a claim has been denied due to a lack of information or the need for additional documentation to process the claim. This code is part of a broader set of denial codes established by insurance companies and billing agencies to standardize the reasons for claim denials. By using these codes, insurance companies can efficiently communicate the reasons for denial, allowing healthcare providers to address the issues and resubmit the claims.
Causes of CO 4 Denial Code
Several factors can lead to a claim being denied with the CO 4 Denial Code. These include:
Insufficient Documentation: If the healthcare provider fails to submit all necessary documentation to support the claim, the insurance company may deny the claim with a CO 4 code. This documentation could include medical records, test results, or any other information that substantiates the medical necessity of the treatment provided.
Lack of Detail: Claims lacking detailed information about the services provided, such as specific codes for procedures or diagnoses, can be denied. The insurance company needs precise details to assess the validity and medical necessity of the claim.
Incorrect or Incomplete Patient Information: Errors in patient demographics or insurance details can lead to a denial. It is crucial that all information provided is accurate and up-to-date to avoid unnecessary denials.
Implications for Healthcare Providers
For healthcare providers, receiving a CO 4 Denial Code can have significant implications. It not only delays reimbursement for services provided but also increases administrative costs associated with appealing the denial and resubmitting the claim. Furthermore, repeated denials can strain relationships between healthcare providers and insurance companies, potentially affecting future claims and the provider’s reputation.
Strategies for Appealing CO 4 Denial Code
Appealing a CO 4 Denial Code requires a thorough understanding of the reason for the denial and the necessary steps to rectify the situation. Here are some strategies healthcare providers can use:
Review the Denial Notice: Carefully examine the denial notice to understand the specific reasons for the CO 4 code. Insurance companies typically provide a detailed explanation or reference a specific section of the policy that justifies the denial.
Gather Necessary Documentation: Once the healthcare provider understands what additional information is required, they should gather all necessary documentation. This could involve retrieving medical records, obtaining additional test results, or clarifying patient information.
Submit an Appeal: With the required documentation in hand, the healthcare provider should submit an appeal to the insurance company. The appeal should clearly address the reasons for the initial denial and provide the requested information. It’s also beneficial to include a cover letter explaining the appeal and highlighting the new information provided.
Follow Up: After submitting the appeal, it’s crucial to follow up with the insurance company. This ensures that the appeal is being processed and can help resolve any further issues promptly.
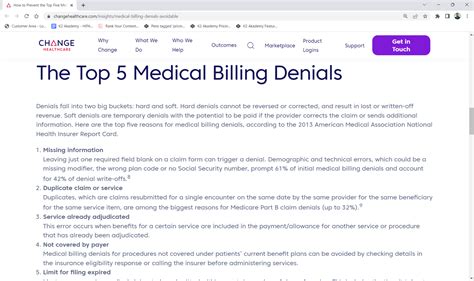
Prevention Strategies
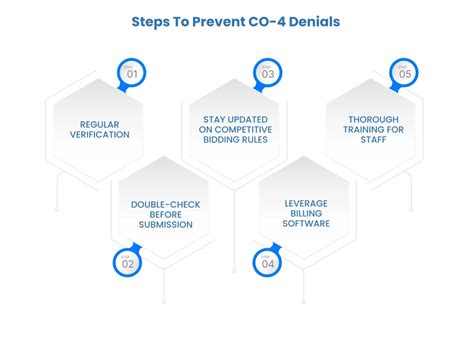
While appealing a CO 4 Denial Code is possible, preventing such denials in the first place is more efficient and cost-effective. Here are some prevention strategies:
Ensure Accurate and Complete Information: Healthcare providers should verify that all claims submitted have complete and accurate patient and service information. This includes double-checking patient demographics, insurance details, and the specifics of the services provided.
Maintain Detailed Records: Keeping detailed medical records and ensuring that all relevant documentation is submitted with the claim can prevent denials due to lack of information.
Train Staff: Continuous training for staff on the importance of accurate and detailed claim submission, as well as on the latest billing and coding regulations, can significantly reduce the incidence of CO 4 denials.
Conclusion
The CO 4 Denial Code is a significant obstacle in the medical billing process, but understanding its causes and how to appeal or prevent it can streamline healthcare operations and improve revenue cycle management. By adopting proactive strategies to ensure complete and accurate claim submissions, healthcare providers can reduce denials, minimize administrative burdens, and foster smoother relationships with insurance companies. This not only benefits the healthcare providers but also enhances patient care by reducing delays in treatment due to billing issues.
Expert Insight: One of the underappreciated aspects of managing CO 4 Denial Codes is the role of technology. Implementing advanced billing software that can automatically verify patient information and flag potential issues before claim submission can significantly reduce denials. Moreover, these systems can help in tracking appeals and follow-ups, making the process more efficient.
FAQ Section
What is the CO 4 Denial Code, and how does it affect medical billing?
+The CO 4 Denial Code is used by insurance companies to denote that a claim has been denied due to insufficient information or the need for additional documentation. It can significantly affect medical billing by delaying reimbursement and increasing administrative costs for healthcare providers.
How can healthcare providers prevent CO 4 Denial Codes?
+Healthcare providers can prevent CO 4 Denial Codes by ensuring that all claims have complete and accurate patient and service information, maintaining detailed medical records, and providing continuous training to staff on billing and coding regulations.
What steps should be taken to appeal a CO 4 Denial Code?
+To appeal a CO 4 Denial Code, healthcare providers should review the denial notice, gather the necessary documentation, submit a detailed appeal, and follow up with the insurance company to ensure the appeal is processed promptly.
In conclusion, understanding and navigating the CO 4 Denial Code is crucial for efficient medical billing and reimbursement processes. By grasping the reasons behind these denials and implementing strategies for prevention and appeal, healthcare providers can enhance their revenue cycle management, reduce administrative burdens, and ultimately focus more on delivering high-quality patient care.