Diabetes Glucose Control: Master Your Levels
Achieving optimal glucose control is a cornerstone of diabetes management, impacting not only the quality of life but also the long-term health outcomes of individuals with diabetes. The importance of maintaining blood glucose levels within a target range cannot be overstated, as it helps prevent the onset of complications associated with diabetes, such as cardiovascular disease, kidney damage, and nerve damage. In this comprehensive guide, we will delve into the intricacies of glucose control, exploring the latest strategies, technologies, and lifestyle adjustments that can help individuals master their glucose levels.
Understanding Blood Glucose Levels
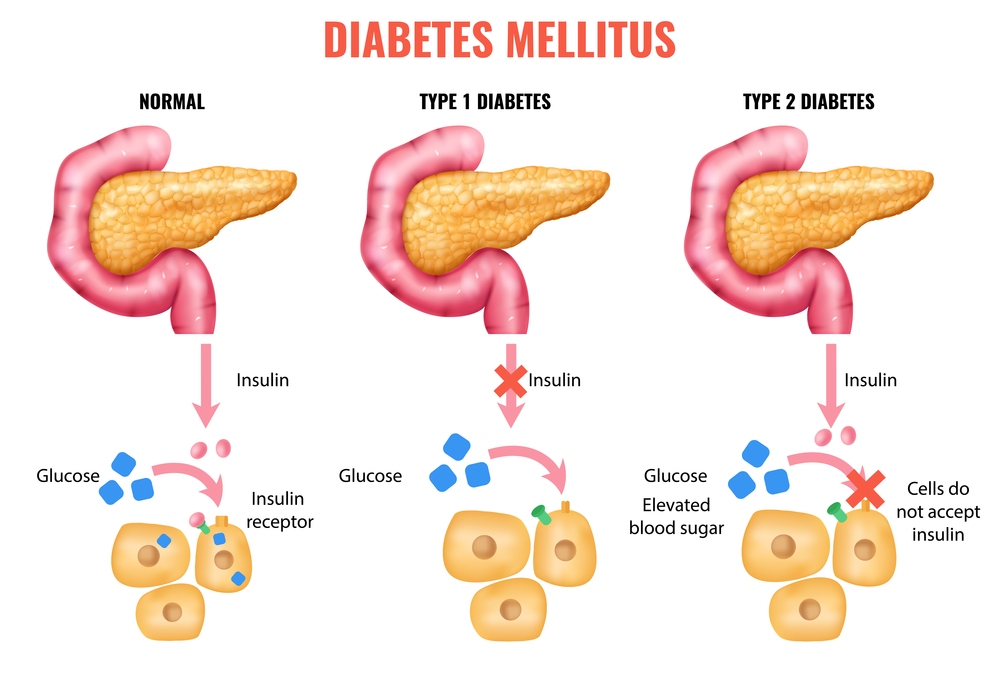
To effectively manage diabetes, it’s crucial to understand what blood glucose levels are and how they are measured. Blood glucose, or blood sugar, refers to the amount of glucose present in the blood. Glucose is a simple sugar that serves as the primary source of energy for the body’s cells. In individuals without diabetes, the body naturally regulates blood glucose levels through the production of insulin, a hormone made by the pancreas that facilitates the entry of glucose into cells.
For people with diabetes, whether it be Type 1, where the body does not produce insulin, or Type 2, where the body does not use insulin properly, managing blood glucose levels is a daily challenge. The goal is to keep blood glucose levels as close to the target range as possible, which typically means:
- Before meals: 70 to 130 mg/dL
- After meals: Less than 180 mg/dL
Strategies for Glucose Control
Effective glucose control involves a multifaceted approach that includes lifestyle modifications, meal planning, physical activity, and, when necessary, medication. Here’s a breakdown of key strategies:
Lifestyle Modifications
- Monitoring Blood Glucose: Regularly checking blood glucose levels helps identify patterns and understand how different factors (like food, exercise, and stress) affect glucose levels.
- Healthy Eating: Focusing on a balanced diet that is low in added sugars, saturated fats, and sodium, and high in fiber, vitamins, and minerals. The Mediterranean Diet and the DASH Diet are often recommended.
- Physical Activity: Engaging in regular physical activity, such as walking, can help lower blood glucose levels and improve insulin sensitivity. Aim for at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous aerobic activity, or a combination of both, per week.
- Stress Management: High levels of stress can elevate cortisol levels, contributing to higher blood glucose. Practices like yoga, meditation, and deep breathing exercises can help manage stress.
Medication and Technology
- Insulin Therapy: For individuals with Type 1 diabetes and some with Type 2, insulin injections or an insulin pump may be necessary to control blood glucose levels.
- Oral Medications: Several types of medications can help manage blood glucose levels, including metformin, sulfonylureas, and meglitinides, among others.
- Continuous Glucose Monitoring (CGM) Systems: These devices provide real-time glucose readings throughout the day and night, offering valuable insights into glucose trends and patterns.
- Insulin Pumps and Smart Pens: These technologies can simplify insulin delivery, providing more flexibility and precision in dosing.
Mastering Glucose Levels: Advanced Techniques
For those looking to further refine their glucose control, several advanced techniques can be particularly useful:
Time in Range (TIR)
TIR refers to the percentage of time an individual’s glucose levels fall within their target range (typically between 70 and 180 mg/dL). Aim for a TIR of at least 70%, which is associated with better health outcomes.
Basal-Bolus Insulin Regimen
This insulin regimen involves taking a combination of long-acting (basal) insulin to cover background glucose needs and short-acting (bolus) insulin before meals to manage meal-related spikes in glucose levels.
Carbohydrate Counting
This meal planning strategy involves tracking the amount of carbohydrates consumed to predict and manage the impact of meals on blood glucose levels. Carbohydrates have the greatest effect on blood glucose levels.
Physical Activity and Glucose Control
Exercise not only improves insulin sensitivity but can also lower blood glucose levels during and after activity. Understanding how different types of physical activity (aerobic, anaerobic, high-intensity interval training) affect glucose levels can help tailor an exercise plan that complements glucose control strategies.
Overcoming Challenges in Glucose Control
Despite the best efforts, achieving consistent glucose control can be challenging. Common obstacles include:
- Hypoglycemia (Low Blood Sugar): Recognizing the signs (shakiness, dizziness, sweating, hunger, irritability, confusion) and treating hypoglycemia promptly with fast-acting carbohydrates is crucial.
- Hyperglycemia (High Blood Sugar): Managing stress, staying hydrated, and adjusting medication or insulin doses as needed can help mitigate hyperglycemia.
- Emotional Challenges: The psychological impact of living with diabetes should not be underestimated. Seeking support from healthcare providers, support groups, or mental health professionals can be invaluable.
Future of Glucose Control
The landscape of diabetes management is evolving rapidly, with advancements in technology, medication, and our understanding of the disease itself. Emerging trends and innovations include:
- Artificial Pancreas Systems: Automated insulin delivery systems that adjust insulin doses based on real-time glucose data from CGM systems.
- Immunotherapies: Research into treatments that could potentially modify or reverse the autoimmune response in Type 1 diabetes.
- Personalized Medicine: Tailoring treatment plans based on an individual’s genetic profile, lifestyle, and medical history.
Conclusion
Mastering glucose levels is a journey that requires patience, persistence, and a personalized approach. By combining the latest medical advancements with lifestyle modifications and a deep understanding of glucose dynamics, individuals with diabetes can achieve better control over their condition, leading to improved health outcomes and an enhanced quality of life. As research and technology continue to advance, the future of diabetes management holds much promise for more effective, personalized, and empowering care.
FAQs
What are the symptoms of high blood sugar in diabetes?
+Symptoms of high blood sugar (hyperglycemia) can include increased thirst and urination, fatigue, blurred vision, cuts or wounds that are slow to heal, and tingling or numbness in the hands and feet. It’s essential to monitor blood glucose levels regularly and seek medical attention if symptoms persist or worsen.
How does exercise impact blood glucose levels?
+Exercise can significantly lower blood glucose levels by improving insulin sensitivity, which allows glucose to enter the cells more efficiently. The effect of exercise on glucose levels can vary depending on the intensity, duration, and type of activity, as well as the individual’s current glucose level and medication regimen.
What role does diet play in glucose control for diabetes?
+Diet plays a central role in glucose control. A balanced diet that is rich in whole foods, such as vegetables, fruits, whole grains, lean proteins, and healthy fats, can help regulate blood glucose levels. Portion control, carbohydrate counting, and understanding glycemic index can also be useful strategies in meal planning for diabetes management.
How can technology, such as continuous glucose monitoring (CGM), aid in glucose control?
+Continuous glucose monitoring (CGM) systems provide real-time glucose readings, offering insights into glucose trends, patterns, and the impact of food, exercise, and other factors on glucose levels. This information can be used to make informed decisions about insulin dosing, meal planning, and physical activity, leading to more precise and personalized glucose control.