How Do You Get Mastitis
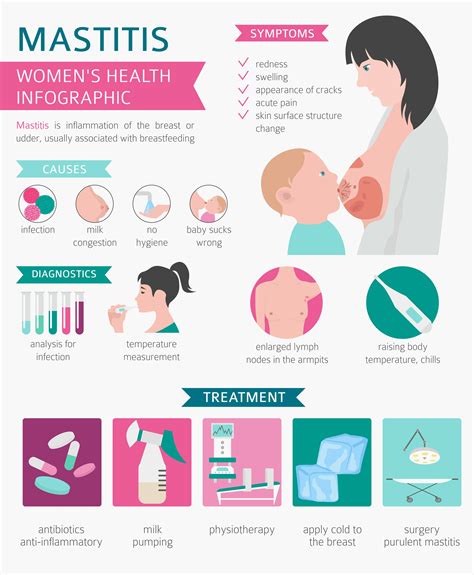
Mastitis is an inflammation of the breast tissue, which can be caused by an infection or other factors. Understanding how mastitis occurs is crucial for prevention and early intervention. The condition is most commonly associated with breastfeeding women, but it can also occur in non-breastfeeding women and, very rarely, in men.
Causes of Mastitis
Infection: The most common cause of mastitis is a bacterial infection, typically caused by Staphylococcus aureus. The bacteria can enter the breast through a crack or sore on the nipple. Breastfeeding mothers are at a higher risk if their baby has a (often temporary) condition called thrush in the mouth, as this fungal infection can be passed back and forth between the baby’s mouth and the mother’s breast.
Plugged Duct: A plugged duct can also lead to mastitis. This happens when one of the milk ducts in the breast becomes blocked, causing milk to build up. This can lead to infection if not resolved.
Poor Latch: A poor latch while breastfeeding can cause nipple trauma, which increases the risk of infection. It can also lead to incomplete emptying of the breast, contributing to the risk of a plugged duct and subsequent infection.
Infrequent Feeding or Incomplete Emptying: Going too long between feedings or not fully emptying the breast can lead to engorgement and increase the risk of mastitis.
Weaning Too Quickly: Sudden weaning or a significant reduction in the frequency of breastfeeding can lead to engorgement and potentially cause mastitis.
previous Mastitis or Breast Surgery: Women who have had mastitis before or those who have undergone breast surgery may have a higher risk.
Immune System Suppression: Certain conditions or medications that suppress the immune system can increase the risk of developing mastitis.
Risk Factors
While mastitis can occur in anyone, certain factors increase the risk, including:
- Breastfeeding: As mentioned, breastfeeding mothers are at a higher risk, especially in the first few weeks.
- Previous History of Mastitis: Women who have had mastitis before are more likely to develop it again.
- Poor Breastfeeding Technique: This can lead to nipple soreness and trauma, increasing the risk of infection.
- Cracked Nipples: Open sores on the nipples provide an easy entry point for bacteria.
- Engorgement: Overly full breasts can lead to plugged ducts and increase the risk of infection.
- Stress and Fatigue: Being overly stressed or fatigued can weaken the immune system, making it harder for the body to fight off infections.
Prevention
Preventing mastitis involves a combination of good breastfeeding practices, self-care, and knowing the early signs of mastitis. Measures include:
- Proper Breastfeeding Technique: Ensure a good latch to prevent nipple trauma.
- Frequent Feeding: Regular, frequent feeding can help prevent engorgement.
- Expressing Milk: Regularly expressing milk can help if the baby is not feeding effectively or if the mother needs to skip a feeding.
- Staying Hydrated: Drinking plenty of water can help with milk production and overall health.
- Getting Enough Rest: Prioritizing rest can help the immune system function well.
Conclusion
Mastitis is a treatable condition, and understanding its causes and risk factors can help in prevention and early detection. If symptoms persist or worsen, it’s essential to consult a healthcare provider for proper diagnosis and treatment, which may include antibiotics for bacterial infections. With proper care and attention, most women can recover from mastitis and continue to breastfeed successfully.
How common is mastitis among breastfeeding women?
+Mastitis is relatively common among breastfeeding women, affecting up to 10% of mothers, though the actual incidence can vary. It typically occurs within the first 6 weeks postpartum but can happen at any time during breastfeeding.
Can mastitis occur in women who are not breastfeeding?
+Yes, though it is much less common. Non-breastfeeding women can develop mastitis due to other conditions such as ductal ectasia, where the ducts beneath the nipple become widened and possibly infected, or periareolar abscesses, which are collections of pus that form in the tissue around the areola.
What are the first signs of mastitis?
+The first signs of mastitis often include a painful area of the breast that may be red, swollen, and warm to the touch. Women may also experience flu-like symptoms such as fever, chills, and a general feeling of being unwell. It's crucial to seek medical attention if these symptoms develop to ensure early treatment and prevent complications.
In conclusion, while mastitis is a concerning condition, understanding its causes, recognizing its symptoms early, and adopting preventive measures can significantly reduce its impact and ensure a successful breastfeeding experience for those who choose to breastfeed.