Diabetic Blood Glucose Levels
Maintaining optimal blood glucose levels is crucial for individuals with diabetes to prevent complications and ensure overall health. Blood glucose levels, also known as blood sugar levels, refer to the amount of glucose present in the blood at a given time. Glucose is a simple sugar that serves as the primary source of energy for the body’s cells. In individuals with diabetes, the body either cannot produce enough insulin (a hormone that regulates blood glucose levels) or cannot effectively use the insulin it produces, leading to elevated blood glucose levels.
Understanding Blood Glucose Levels
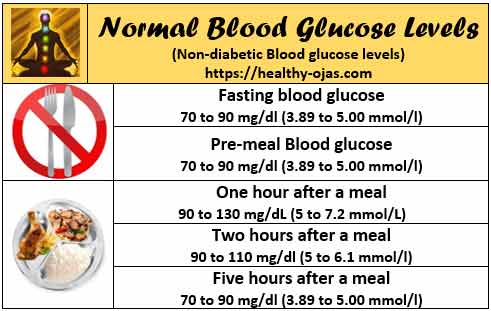
Normal blood glucose levels typically range from 70 to 140 mg/dL (milligrams per deciliter) throughout the day, with levels usually being at their lowest in the morning after an overnight fast. However, these levels can fluctuate based on various factors such as diet, physical activity, and the timing of medication or insulin doses. Individuals with diabetes often have blood glucose levels outside of this normal range, which can lead to both short-term and long-term health issues.
Impact of High Blood Glucose Levels
High blood glucose levels, or hyperglycemia, can occur due to several reasons including overeating, particularly consuming foods high in sugar and carbohydrates, skipping doses of diabetes medication or insulin, being less active than usual, and experiencing stress or illness. Hyperglycemia can lead to symptoms such as increased thirst and urination, fatigue, blurred vision, slow healing of cuts and wounds, and frequent infections. If left unmanaged, high blood glucose levels over time can result in serious complications such as heart disease, kidney damage, nerve damage, and vision problems, including blindness.
Importance of Monitoring Blood Glucose Levels
Regular monitoring of blood glucose levels is essential for managing diabetes effectively. This can be done through a fingerstick test using a glucometer, which provides immediate feedback on blood glucose levels. Additionally, some individuals use continuous glucose monitors (CGMs) that provide real-time data on glucose levels throughout the day and night. Monitoring helps in identifying patterns of high or low blood glucose levels, allowing for adjustments in diet, exercise, and medication to maintain levels within a target range.
Strategies for Managing Blood Glucose Levels
Several strategies can help in managing blood glucose levels:
Dietary Changes: Following a balanced diet that is low in added sugars, saturated fats, and sodium, and high in fiber, fruits, vegetables, and whole grains can help regulate blood glucose levels.
Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, along with muscle-strengthening activities on 2 or more days a week, can improve insulin sensitivity and lower blood glucose levels.
Medication Adherence: Taking diabetes medications or insulin as prescribed by a healthcare provider is crucial. Medications can help lower blood glucose levels by stimulating insulin release, reducing glucose production in the liver, or improving the body’s use of insulin.
Stress Management: Practicing stress-reducing techniques such as yoga, meditation, or deep breathing exercises can help manage stress, which can otherwise raise blood glucose levels.
Regular Health Check-ups: Regular visits to healthcare providers can help monitor the progression of diabetes and the effectiveness of the management plan, allowing for timely adjustments to maintain optimal blood glucose levels.
Advanced Technologies for Blood Glucose Management
The management of blood glucose levels has become more efficient with the advent of advanced technologies. Continuous glucose monitoring systems, insulin pumps, and smart insulin pens are some of the tools that provide real-time data and automated insulin delivery, making it easier for individuals with diabetes to maintain their blood glucose levels within a healthy range. Mobile applications also play a significant role in tracking diet, exercise, and medication adherence, offering personalized advice and reminders to support diabetes management.
Addressing Common Misconceptions
Despite the advancements in diabetes management, several misconceptions prevail. For instance, many believe that diabetes is solely caused by eating too much sugar, which oversimplifies the complex interplay of genetic, environmental, and lifestyle factors that contribute to the development of the disease. Another misconception is that individuals with diabetes must follow a very restrictive diet, which, while it’s true that diet plays a crucial role, the focus should be on balanced and sustainable eating habits rather than extreme dietary restrictions.
Future Directions in Diabetes Management
The future of diabetes management holds promise with ongoing research into new medications, insulin delivery systems, and technologies aimed at improving the quality of life for individuals with diabetes. Stem cell therapies, islet cell transplantation, and the development of an artificial pancreas are among the potential breakthroughs that could revolutionize diabetes care. Furthermore, advances in personalized medicine and genetic research may lead to more targeted and effective treatment strategies tailored to an individual’s specific needs and genetic profile.
Conclusion
Managing diabetic blood glucose levels requires a comprehensive approach that includes dietary adjustments, regular physical activity, adherence to medication regimens, and the utilization of advanced technologies. By understanding the importance of blood glucose control and leveraging the available tools and strategies, individuals with diabetes can lead active, healthy lives while minimizing the risk of diabetes-related complications. As research continues to unravel the complexities of diabetes, it is essential for healthcare providers, individuals with diabetes, and their families to stay informed and adapt to the evolving landscape of diabetes management.
What are the normal blood glucose levels for individuals without diabetes?
+Normal blood glucose levels are typically between 70 to 140 mg/dL throughout the day, with levels usually being at their lowest in the morning after an overnight fast.
How often should individuals with diabetes check their blood glucose levels?
+The frequency of checking blood glucose levels can vary depending on the type of diabetes, the treatment plan, and the individual’s health status. Generally, it is recommended to check levels at least four times a day, including before meals and before bedtime, but this can be adjusted based on specific guidance from a healthcare provider.
What are the risks of unmanaged high blood glucose levels?
+Unmanaged high blood glucose levels can lead to serious complications, including heart disease, kidney damage, nerve damage, and vision problems. It is crucial to manage blood glucose levels through a combination of diet, exercise, and, if necessary, medication or insulin therapy.
Can lifestyle changes alone manage diabetes?
+Lifestyle changes, including dietary adjustments and increased physical activity, are fundamental in managing diabetes. For some individuals, particularly those with type 2 diabetes, lifestyle changes alone may be sufficient to manage the condition. However, many people will also require medication or insulin therapy to achieve and maintain target blood glucose levels.
How does stress affect blood glucose levels?
+Stress can raise blood glucose levels by triggering the release of stress hormones like cortisol, which can cause the liver to release stored glucose (glycogen) into the bloodstream. Additionally, stress can lead to poor food choices and decreased physical activity, further exacerbating the issue.
What role does technology play in managing diabetes?
+Technology plays a significant role in managing diabetes, from continuous glucose monitoring systems and insulin pumps to mobile applications that track dietary intake, physical activity, and medication adherence. These tools can provide real-time data, automate certain aspects of diabetes care, and offer personalized advice to support better management of the condition.