Diabetic Blood Sugar Levels
Living with diabetes requires a deep understanding of how to manage blood sugar levels effectively. The intricacies of blood glucose management can be daunting, especially for those newly diagnosed. It’s essential to grasp the fundamentals of diabetic blood sugar levels, including what constitutes normal levels, how to measure them, and the strategies for maintaining control.
Understanding Blood Sugar Levels
Blood sugar, or glucose, is the primary energy source for the body’s cells. In individuals with diabetes, the body either doesn’t produce enough insulin (Type 1 diabetes) or cannot effectively use the insulin it produces (Type 2 diabetes), leading to elevated blood glucose levels. Over time, high blood sugar can lead to serious health complications, including heart disease, kidney failure, and nerve damage.
Normal Blood Sugar Levels
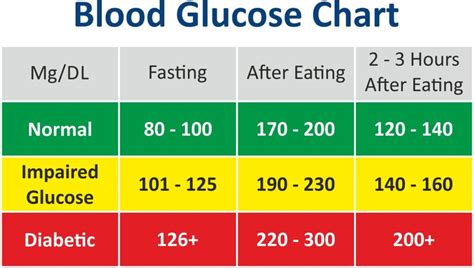
For people without diabetes, normal blood sugar levels are typically between 70 to 99 mg/dL when fasting (not having eaten for at least 8 hours) and less than 140 mg/dL two hours after eating. In individuals with diabetes, the target blood sugar levels are slightly different:
- Fasting Blood Sugar: 80 to 130 mg/dL
- Before Meals: Less than 130 mg/dL
- After Meals (1-2 hours): Less than 180 mg/dL
Achieving these targets can significantly reduce the risk of diabetes-related complications.
Measuring Blood Sugar Levels
The most common method for measuring blood sugar levels is through a fingerstick test using a glucometer. This involves pricking the finger with a lancet to draw a small drop of blood, which is then placed on a test strip inserted into the glucometer. The device provides a reading of the current blood glucose level.
Continuous Glucose Monitors (CGMs) offer another option, providing real-time and historical glucose data through a small sensor inserted under the skin. While traditionally prescribed for individuals with Type 1 diabetes, CGMs are increasingly recommended for those with Type 2 diabetes, especially those on insulin therapy or experiencing significant glucose variability.
Strategies for Managing Blood Sugar Levels
Effective management of blood sugar levels involves a multifaceted approach, including diet, exercise, medication, and monitoring.
Dietary Management: Focus on consuming a balanced diet that is low in added sugars, saturated fats, and sodium. Emphasize whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats. For some, working with a registered dietitian or a certified diabetes educator can help tailor a diet plan to individual needs.
Physical Activity: Regular physical activity helps lower blood sugar levels and improves insulin sensitivity. Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous aerobic exercise per week, along with strength-training activities at least twice a week.
Medication Adherence: For those prescribed medication or insulin, taking these as directed is crucial. Medications may include metformin, sulfonylureas, or other oral medications, and various types of insulin for those who require it.
Stress Management: Chronic stress can elevate blood sugar levels. Engaging in stress-reducing activities such as yoga, meditation, or deep breathing exercises can help manage stress.
Regular Monitoring: Regularly checking blood sugar levels helps understand how different factors (like food, exercise, and stress) affect glucose levels. This information can guide adjustments in the management plan.
Challenges and Complications
Despite the best efforts, managing blood sugar levels can be challenging, and complications can arise. Hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) are common issues that require immediate attention.
Hypoglycemia: Symptoms include shakiness, dizziness, sweating, hunger, irritability, confusion, or even loss of consciousness in severe cases. Treatment involves consuming fast-acting carbohydrates like glucose tablets, juice, or regular soda, followed by a snack with protein to help stabilize glucose levels.
Hyperglycemia: High blood sugar can lead to symptoms such as increased thirst and urination, blurred vision, fatigue, and in severe cases, diabetic ketoacidosis (DKA) or hyperglycemic hyperosmolar nonketotic syndrome (HHNS), both of which are medical emergencies.
Innovations in Diabetes Management
The field of diabetes management is rapidly evolving, with new technologies and treatments being developed. Advances in CGMs, insulin pumps, and automated insulin delivery systems are making it easier for individuals to manage their blood sugar levels. Additionally, research into new medications and even potential cures, such as stem cell therapies and islet cell transplants, offers hope for the future.
Conclusion
Managing diabetic blood sugar levels is a complex but manageable task. By understanding normal blood sugar ranges, effectively using measurement tools, and implementing a comprehensive management plan that includes diet, exercise, medication, and stress management, individuals with diabetes can lead healthy, active lives. Staying informed about the latest developments in diabetes care and working closely with healthcare providers are key components of successful blood sugar management.
What are the risks of not managing blood sugar levels effectively?
+Not managing blood sugar levels effectively can lead to serious health complications, including heart disease, kidney failure, nerve damage, and vision problems. High blood sugar over time can also lead to conditions like diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar nonketotic syndrome (HHNS), which are medical emergencies.
How often should I check my blood sugar levels?
+The frequency of checking blood sugar levels depends on the type of diabetes, the treatment plan, and the individual’s lifestyle. Generally, those with Type 1 diabetes or those using insulin may need to check their levels more frequently (up to 4-6 times a day) than those with Type 2 diabetes managed through diet and oral medications.
Can diet and exercise alone manage blood sugar levels?
+For some individuals with Type 2 diabetes, especially those recently diagnosed, managing blood sugar levels through diet and exercise may be possible. However, this depends on the severity of the diabetes, the individual’s overall health, and how well they can adhere to lifestyle changes. Often, a combination of diet, exercise, and medication (including insulin) is necessary to achieve and maintain target blood sugar levels.