Glucose Control Guide: Optimal Levels
Maintaining optimal glucose levels is crucial for overall health, particularly for individuals with diabetes or those at risk of developing the condition. Glucose, a simple sugar, serves as the primary source of energy for cells throughout the body. When glucose levels are properly managed, it helps prevent complications associated with diabetes, such as heart disease, kidney damage, and nerve damage. In this comprehensive guide, we will delve into the importance of glucose control, the optimal glucose levels, and strategies for achieving and maintaining these levels.
Understanding Glucose and Its Role in the Body
Before diving into glucose control, it’s essential to understand glucose’s role in the body. Glucose is absorbed into the bloodstream after consuming carbohydrates, which are broken down into glucose during digestion. The pancreas, an organ located behind the stomach, produces insulin, a hormone that regulates blood glucose levels. Insulin facilitates the entry of glucose into cells, where it is used for energy production, growth, and repair. In individuals with diabetes, the body either doesn’t produce enough insulin (Type 1 diabetes) or cannot effectively use the insulin it produces (Type 2 diabetes), leading to elevated blood glucose levels.
Optimal Glucose Levels
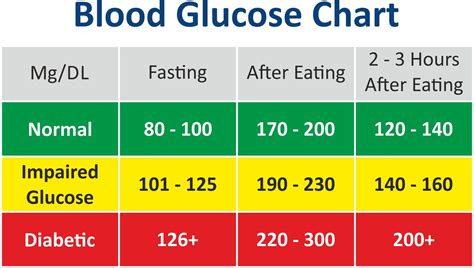
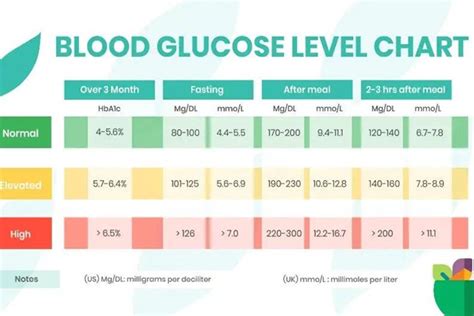
Optimal glucose levels vary slightly throughout the day, particularly in response to meals. The American Diabetes Association (ADA) provides guidelines for optimal glucose levels:
- Fasting glucose levels should be less than 100 mg/dL for people without diabetes and less than 130 mg/dL for those with diabetes.
- Postprandial (after meal) glucose levels should be less than 140 mg/dL for people without diabetes and less than 180 mg/dL for those with diabetes.
Achieving and maintaining these levels requires a combination of diet, exercise, and, for some, medication.
Strategies for Glucose Control
Dietary Management
Diet plays a crucial role in glucose control. Here are some dietary strategies:
- Choose complex carbohydrates: Foods like whole grains, fruits, and vegetables are rich in fiber, which slows down the absorption of glucose into the bloodstream, preventing sudden spikes.
- Include protein and healthy fats: Protein and healthy fats, found in foods like lean meats, fish, avocados, and nuts, can help regulate appetite and slow gastric emptying, reducing the impact on blood glucose levels.
- Limit added sugars and refined carbohydrates: Foods high in added sugars and refined carbohydrates can cause significant spikes in blood glucose levels.
Physical Activity
Regular physical activity is another key component of glucose control:
- Aerobic exercise: Activities like walking, cycling, and swimming improve insulin sensitivity, helping the body to more effectively use insulin.
- Resistance training: Building muscle through resistance exercises can further enhance insulin sensitivity and glucose uptake into muscles.
Monitoring and Medication
For many individuals, especially those with diabetes, monitoring blood glucose levels and adjusting medication as needed is crucial:
- Regular blood glucose monitoring: This helps identify patterns and make informed decisions about diet, exercise, and medication.
- Adherence to medication: For those requiring medication, taking it as prescribed by a healthcare provider is essential for maintaining optimal glucose levels.
Advanced Glucose Monitoring Technologies
Recent advancements in glucose monitoring technologies have made it easier for individuals to track their glucose levels continuously and make data-driven decisions:
- Continuous Glucose Monitors (CGMs): These small devices attach to the body and provide real-time glucose level readings throughout the day and night.
- Flash Glucose Monitors: Similar to CGMs, these devices provide on-demand glucose readings with a quick scan over the sensor.
Lifestyle Adjustments for Long-Term Glucose Control
Maintaining optimal glucose levels is a long-term commitment that requires consistent lifestyle adjustments:
- Stress management: High levels of stress can affect blood glucose levels. Engaging in stress-reducing activities like yoga, meditation, or deep breathing exercises can help.
- Sleep and glucose control: Getting adequate sleep is crucial, as poor sleep quality and duration can negatively affect insulin sensitivity and glucose control.
- Regular health check-ups: Regular visits to a healthcare provider can help monitor progress, adjust treatment plans as needed, and prevent complications.
Conclusion
Achieving and maintaining optimal glucose levels is a multifaceted approach that involves dietary changes, regular physical activity, monitoring, and when necessary, medication. By understanding the role of glucose in the body, setting realistic goals, and making consistent lifestyle adjustments, individuals can effectively manage their glucose levels, reducing the risk of diabetes-related complications and improving overall health and wellbeing.
What are the optimal fasting glucose levels for individuals with diabetes?
+For individuals with diabetes, optimal fasting glucose levels should be less than 130 mg/dL. However, it’s crucial to follow the specific targets set by your healthcare provider, as these can vary based on age, other health conditions, and the risk of hypoglycemia.
How often should I monitor my blood glucose levels if I have diabetes?
+The frequency of blood glucose monitoring depends on the type of diabetes, treatment plan, and individual factors such as risk of hypoglycemia. Generally, individuals with Type 1 diabetes or those using insulin may need to test more frequently (up to 4-6 times a day) than those with Type 2 diabetes managed through diet and oral medications.
Can lifestyle changes alone control blood glucose levels, or is medication always necessary?
+Lifestyle changes, including diet and exercise, can significantly impact blood glucose control. For individuals with prediabetes or newly diagnosed Type 2 diabetes, lifestyle changes may be sufficient to manage glucose levels. However, for many, especially those with Type 1 diabetes or advanced Type 2 diabetes, medication is necessary to achieve and maintain optimal glucose levels. The decision should be made in consultation with a healthcare provider.