Glucose Level Control: Master Your Numbers

Maintaining optimal glucose levels is a delicate balancing act, crucial for overall health, particularly for individuals managing diabetes. The consequences of uncontrolled glucose levels can be severe, ranging from immediate symptoms like blurry vision and frequent urination to long-term complications such as cardiovascular disease and kidney damage. Understanding how to master glucose levels involves a deep dive into the physiology of glucose metabolism, the impact of lifestyle choices, and the strategic use of medical interventions.
The Physiology of Glucose Metabolism
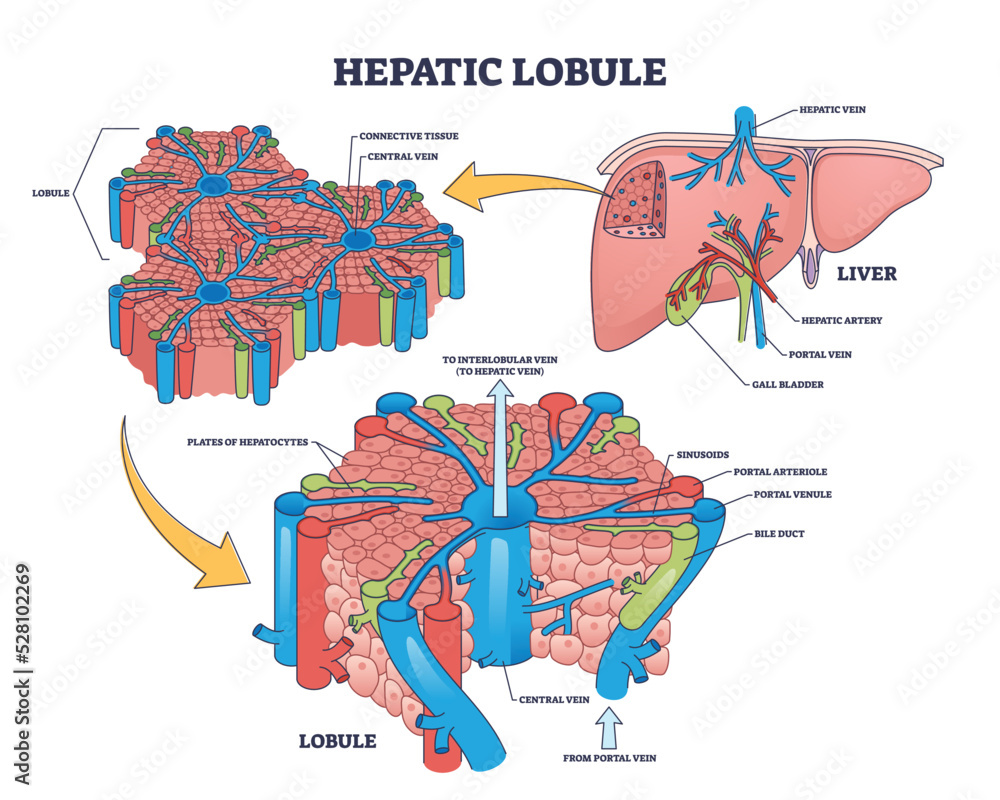
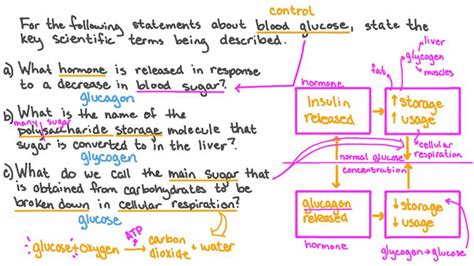
Glucose, a simple sugar, is the primary source of energy for the body’s cells. Its metabolism is tightly regulated by a complex interplay of hormones, primarily insulin and glucagon, both produced by the pancreas. Insulin lowers blood glucose levels by facilitating the entry of glucose into cells, where it can be used for energy, stored as glycogen, or converted to fat for longer-term storage. Conversely, glucagon raises blood glucose levels by stimulating the liver to release stored glucose (glycogen) into the bloodstream and promoting the production of glucose from non-carbohydrate sources (gluconeogenesis).
Lifestyle Choices: The Cornerstone of Glucose Control
Lifestyle modifications are foundational in managing glucose levels. These include dietary changes, physical activity, stress management, and adequate sleep.
Dietary Adjustments: Focus on consuming a balanced diet that is rich in whole, unprocessed foods such as vegetables, fruits, whole grains, lean proteins, and healthy fats. These foods are typically high in fiber and low in added sugars, which can help regulate blood glucose levels. Additionally, understanding the glycemic index (GI) of foods can help in making informed choices; foods with a lower GI cause a slower and smaller rise in blood glucose levels.
Physical Activity: Regular physical activity improves the body’s ability to use insulin and can lower blood glucose levels. Both aerobic exercises (such as walking, swimming) and resistance training (like weightlifting) are beneficial, with the added advantage of improving overall health and reducing the risk of heart disease.
Stress Management: Chronic stress can raise blood glucose levels and worsen diabetes management. Engaging in stress-reducing activities such as yoga, meditation, or deep breathing exercises can help mitigate this effect.
Adequate Sleep: Getting enough sleep is crucial for glucose regulation. Poor sleep quality and duration can lead to insulin resistance, a precursor to type 2 diabetes. Aim for 7-8 hours of sleep per night.
Medical Interventions: When and How
For many individuals, particularly those with diabetes, lifestyle changes alone may not be sufficient to maintain optimal glucose levels, necessitating the use of medications or insulin therapy.
Oral Medications: Various classes of drugs are available to manage diabetes, including metformin, sulfonylureas, and DPP-4 inhibitors, among others. Each works through different mechanisms to improve insulin sensitivity, reduce glucose production in the liver, or enhance insulin secretion.
Insulin Therapy: Insulin is indispensable for individuals with type 1 diabetes and many with advanced type 2 diabetes. It can be administered via injections or an insulin pump, with the goal of mimicking the body’s natural insulin release as closely as possible.
Monitoring and Technology: Continuous glucose monitoring (CGM) systems and flash glucose monitors provide real-time data on glucose levels, enabling more precise management decisions. Additionally, technologies like insulin pumps and automated insulin delivery systems can offer more flexible and dynamic glucose control.
Practical Application Guides: Converting Theory to Action
- Keep a Food Diary: Recording what you eat and when can help identify patterns and foods that affect your glucose levels.
- Set Realistic Goals: Aim for small, achievable changes in diet and exercise to build sustainable habits.
- Stay Hydrated: Drinking enough water can help prevent dehydration, which can be mistaken for high blood sugar symptoms.
- Regular Check-ups: Regular health check-ups can help monitor progress and adjust management plans as needed.
Future Trends in Glucose Level Control
Advancements in technology and medical science are continually improving diabetes management. Emerging trends include the development of implantable devices that can detect glucose levels and automatically administer insulin, as well as research into new insulins with faster onset and longer duration of action. Furthermore, the integration of artificial intelligence (AI) and machine learning (ML) into glucose monitoring and insulin delivery systems promises more personalized and efficient diabetes care.
Addressing Potential Objections
- “I don’t have time to exercise or cook healthy meals.” Even small increments of physical activity and simple meal preparations can have a significant impact. Find ways to incorporate activity into your daily routine, like taking the stairs or walking to work, and prep meals in advance.
- “I’m overwhelmed by the amount of information on diabetes management.” Start with small, manageable changes and consult with healthcare professionals or diabetes educators for personalized guidance.
Decision Framework: Making Informed Choices
When considering different management strategies, it’s essential to weigh the pros and cons of each approach:
| Strategy | Pros | Cons |
|---|---|---|
| Dietary Changes | Improves overall health, cost-effective | Can be challenging to maintain |
| Physical Activity | Enhances insulin sensitivity, improves mental health | Requires time commitment |
| Medications/Insulin | Rapidly effective, widely available | Can have side effects, requires medical supervision |
Conceptual Exploration: Understanding the Broader Impact
The management of glucose levels intersects with broader health and societal issues. The increasing prevalence of diabetes is a global health concern, influenced by factors such as urbanization, diet, and physical inactivity. Understanding these underlying trends can inform public health initiatives and individual management strategies.
Historical Evolution: Tracing the Development of Diabetes Management
The approach to diabetes management has undergone significant evolution, from the early recognition of the disease in ancient civilizations to the modern arsenal of medications, devices, and lifestyle interventions. This historical context underscores the importance of continued research and innovation in improving glucose level control.
Natural Storytelling Elements: Illustrating Key Concepts
Consider the story of an individual who, after being diagnosed with pre-diabetes, embarked on a journey of lifestyle modification. Through small, incremental changes in diet and physical activity, this person not only prevented the onset of diabetes but also experienced overall improved health and wellbeing. This narrative illustrates the power of proactive management and the potential for positive change.
FAQ Section
What are the symptoms of high blood glucose levels?
+High blood glucose levels can cause symptoms such as increased thirst and urination, blurred vision, fatigue, and cuts or wounds that are slow to heal. If left untreated, it can lead to more severe complications.
How can I prevent diabetes if I have a family history?
+Even with a family history, you can reduce your risk of developing diabetes by maintaining a healthy weight, following a balanced diet, staying physically active, and avoiding tobacco use. Regular health check-ups can also help in early detection and management.
What is the difference between type 1 and type 2 diabetes?
+Type 1 diabetes is an autoimmune condition where the body's immune system attacks the insulin-producing beta cells in the pancreas, requiring insulin therapy for survival. Type 2 diabetes, on the other hand, is characterized by insulin resistance (when the body's cells don't respond to insulin as they should) and impaired insulin secretion, often managed through lifestyle changes and sometimes medication or insulin.
In conclusion, mastering glucose levels is a multifaceted challenge that requires a comprehensive approach, encompassing lifestyle modifications, medical interventions, and a deep understanding of the individual’s unique physiology and circumstances. By leveraging the latest in medical science, technology, and personal commitment, individuals can achieve optimal glucose control, mitigating the risk of diabetes-related complications and enhancing overall quality of life.