Nuchal Translucency Screening
The nuchal translucency (NT) screening is a non-invasive prenatal test used to assess the risk of chromosomal abnormalities, particularly Down syndrome, in a developing fetus. This screening test is typically performed between 11 and 14 weeks of gestation, during the first trimester of pregnancy. The NT screening measures the thickness of the nuchal fold, a fluid-filled space at the back of the fetus’s neck, using high-resolution ultrasound technology.
What is Nuchal Translucency?
Nuchal translucency refers to the sonographic appearance of the subcutaneous tissue between the fetal skin and the soft tissue overlying the cervical spine. Under normal circumstances, this area appears as a thin, hypoechogenic (fluid-filled) space. An increased NT thickness is associated with a higher risk of aneuploidy, particularly Down syndrome (trisomy 21), as well as other chromosomal abnormalities, such as trisomy 18 (Edwards syndrome) and trisomy 13 (Patau syndrome).
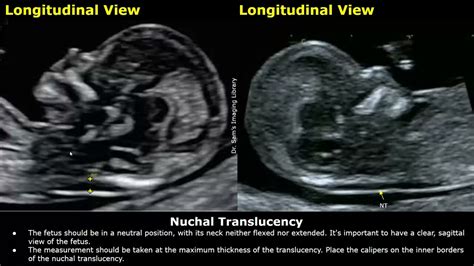
How is the NT Screening Performed?
The NT screening is a relatively simple and quick procedure, taking approximately 30 minutes to complete. The test involves:
- Ultrasound examination: A trained sonographer or obstetrician performs a transabdominal ultrasound to visualize the fetus and measure the NT.
- Fetal measurement: The sonographer measures the fetal crown-rump length (CRL) to confirm gestational age and ensure accurate NT measurement.
- NT measurement: The sonographer measures the thickness of the nuchal fold, typically at the level of the fetal neck, using a standardized technique.
Interpreting NT Results
The NT measurement is interpreted in conjunction with the fetus’s gestational age and other maternal factors, such as age and medical history. An NT thickness of 3.5 mm or greater is generally considered increased and may indicate a higher risk of chromosomal abnormalities. However, it is essential to note that an increased NT does not necessarily mean the fetus has a chromosomal abnormality, but rather that the risk is higher.
Risk Assessment and Next Steps
After the NT screening, the results are combined with other factors, such as:
- Maternal age: The risk of chromosomal abnormalities increases with maternal age.
- Medical history: A history of chromosomal abnormalities in previous pregnancies or family members.
- Biochemical markers: The presence of certain proteins in the maternal blood, such as free beta-hCG and PAPP-A.
The combined results provide an estimated risk of chromosomal abnormalities. If the risk is elevated, the pregnant individual may be offered additional testing, such as:
- Non-invasive prenatal testing (NIPT): A blood test that analyzes cell-free DNA in the maternal bloodstream to detect chromosomal abnormalities.
- Chorionic villus sampling (CVS): A diagnostic test that involves removing a small sample of placental tissue for genetic analysis.
- Amniocentesis: A diagnostic test that involves removing a small sample of amniotic fluid for genetic analysis.
Benefits and Limitations of NT Screening
The NT screening has several benefits, including:
- Early detection: The test can detect increased risk of chromosomal abnormalities early in pregnancy, allowing for informed decision-making.
- Non-invasive: The test is safe and does not pose a risk to the fetus or mother.
- High sensitivity: The NT screening has a high detection rate for Down syndrome, particularly when combined with other markers.
However, the NT screening also has limitations:
- False positives: Some fetuses with increased NT may not have chromosomal abnormalities.
- False negatives: Some fetuses with normal NT may still have chromosomal abnormalities.
- Limited specificity: The NT screening is not specific to Down syndrome and may detect other chromosomal abnormalities.
Conclusion
The nuchal translucency screening is a valuable tool for assessing the risk of chromosomal abnormalities, particularly Down syndrome, during the first trimester of pregnancy. While the test has benefits and limitations, it provides essential information for pregnant individuals and their healthcare providers, allowing for informed decision-making and targeted follow-up testing.
What is the purpose of the nuchal translucency screening?
+The purpose of the nuchal translucency screening is to assess the risk of chromosomal abnormalities, particularly Down syndrome, in a developing fetus during the first trimester of pregnancy.
How accurate is the nuchal translucency screening?
+The nuchal translucency screening has a high detection rate for Down syndrome, particularly when combined with other markers. However, the test is not 100% accurate and may produce false positives or false negatives.
What are the benefits of the nuchal translucency screening?
+The benefits of the nuchal translucency screening include early detection, non-invasiveness, and high sensitivity for detecting chromosomal abnormalities.
What are the limitations of the nuchal translucency screening?
+The limitations of the nuchal translucency screening include false positives, false negatives, and limited specificity for detecting Down syndrome.
What happens if the nuchal translucency screening indicates an increased risk of chromosomal abnormalities?
+If the nuchal translucency screening indicates an increased risk of chromosomal abnormalities, the pregnant individual may be offered additional testing, such as non-invasive prenatal testing, chorionic villus sampling, or amniocentesis.