Glucose Levels In Blood
The management and regulation of glucose levels in the blood is a critical aspect of human health, intricately linked to the body’s metabolic processes. Glucose, a simple sugar, serves as the primary source of energy for cells throughout the body. Its concentration in the blood is tightly regulated by a complex interplay of hormones, primarily insulin and glucagon, which are produced by the pancreas. This regulation is essential to maintain homeostasis and ensure the proper functioning of various bodily systems.
Understanding Blood Glucose Regulation
The pancreas plays a pivotal role in blood glucose regulation. After a meal, as glucose levels in the blood rise, the pancreas releases insulin. Insulin acts like a key, facilitating the entry of glucose into cells, thereby lowering blood glucose levels. Conversely, when blood glucose levels drop, such as during fasting, the pancreas releases glucagon, which stimulates the liver to release stored glucose (glycogen) into the bloodstream, thereby increasing blood glucose levels.
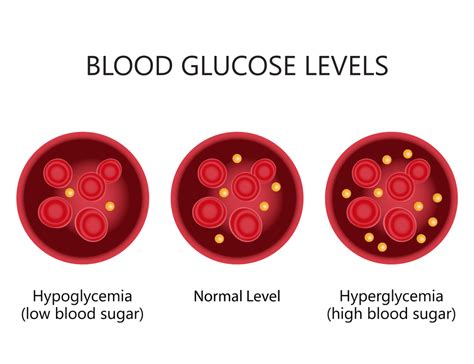
This delicate balance is crucial for preventing both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), conditions that can lead to serious health complications if not managed properly. Hyperglycemia can damage organs and tissues over time, leading to complications such as heart disease, kidney failure, and nerve damage. Hypoglycemia, if severe, can cause confusion, loss of consciousness, and even death.
Factors Influencing Blood Glucose Levels
Several factors can influence blood glucose levels, including diet, physical activity, stress, and certain medications. Consuming foods high in simple carbohydrates can cause a rapid spike in blood glucose, while regular physical activity can enhance the body’s sensitivity to insulin, helping to lower blood glucose levels. Stress triggers the release of stress hormones like cortisol and adrenaline, which can raise blood glucose levels. Certain medications, especially steroids and some psychiatric medications, can also affect blood glucose control.
Monitoring and Management of Blood Glucose
For individuals with diabetes or those at risk of developing the condition, monitoring blood glucose levels is a crucial aspect of disease management. This can be done through various methods, including:
- Fingerstick Glucose Monitoring: The most common method involves pricking the finger with a lancet to collect a small blood sample, which is then placed on a test strip and read by a glucose meter.
- Continuous Glucose Monitoring (CGM) Systems: These systems involve wearing a small sensor under the skin, typically on the abdomen or arm, which continuously measures glucose levels throughout the day and night.
- Flash Glucose Monitoring: Similar to CGM, but does not require a separate receiver; instead, the sensor is scanned with a reader or a compatible smartphone to get the current glucose level and trend.
Maintaining Healthy Blood Glucose Levels
Maintaining healthy blood glucose levels involves a multifaceted approach that includes dietary modifications, regular physical activity, stress management, and, when necessary, medication. Dietary recommendations often emphasize whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats. Regular physical activity, such as walking, can significantly improve insulin sensitivity. Managing stress through techniques like yoga, meditation, or deep breathing exercises can also help regulate blood glucose levels.
Future Directions in Blood Glucose Management
The future of blood glucose management holds promise with emerging technologies and therapeutic approaches. Advances in CGM systems and insulin pumps are making diabetes management more automated and efficient. The development of smart insulin pens and patches that can automatically adjust insulin delivery based on real-time glucose levels is also on the horizon. Furthermore, research into new medications and therapeutic strategies, such as stem cell therapies aimed at regenerating pancreatic beta cells, offers hope for improved or even reversed diabetes outcomes.
Conclusion
The regulation of blood glucose levels is a vital process that underscores the intricate balance and resilience of the human body. Through a deep understanding of the factors that influence glucose metabolism and the adoption of healthy lifestyle choices, individuals can play an active role in maintaining optimal blood glucose levels. As medical science continues to evolve, the tools and strategies available for managing blood glucose will likely become more sophisticated, offering new avenues for the prevention and treatment of diabetes and related metabolic disorders.
What are normal blood glucose levels?
+Normal blood glucose levels are typically considered to be between 70 to 140 mg/dL, though these can vary slightly depending on the timing of the last meal and individual health status.
How often should I check my blood glucose levels if I have diabetes?
+The frequency of checking blood glucose levels can vary depending on the type of diabetes and the treatment plan. Generally, individuals with type 1 diabetes and some with type 2 diabetes may need to check their levels multiple times a day, especially before meals and before bedtime, and occasionally during the night.
Can diet and exercise alone manage blood glucose levels for someone with diabetes?
+For some individuals, especially those with prediabetes or newly diagnosed type 2 diabetes, lifestyle modifications including diet and exercise can be effective in managing blood glucose levels. However, this depends on the severity of the diabetes, individual health factors, and how well these changes are implemented and maintained.