Neomycin And Polymyxin
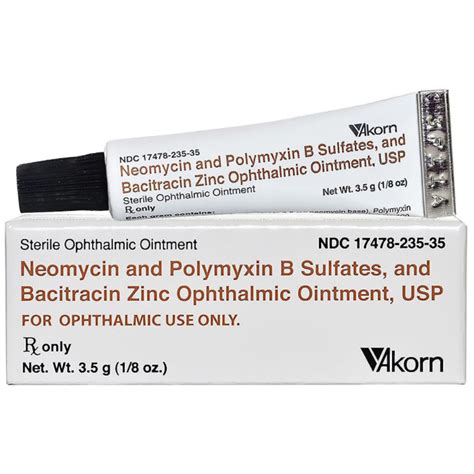
The combination of neomycin and polymyxin is a potent antibiotic formulation used to treat various bacterial infections, particularly those affecting the eyes, ears, and skin. This dual-antibiotic combination is designed to provide broad-spectrum coverage against both Gram-positive and Gram-negative bacteria, making it a widely used and effective treatment option for infections such as conjunctivitis, otitis externa, and minor skin infections.
Historical Evolution of Neomycin and Polymyxin
Neomycin and polymyxin are both discovered products of the mid-20th century, a period rich with advancements in antibiotic research. Neomycin, an aminoglycoside antibiotic, was first isolated in 1949 from the actinomycete Streptomyces fradiae. Its discovery marked an important milestone in the treatment of bacterial infections, offering a new avenue for combating diseases caused by Gram-negative bacteria. Polymyxin, on the other hand, is a group of bactericidal antibiotics derived from Bacillus polymyxa. The first polymyxin, polymyxin A, was introduced in the early 1950s, followed by other variants, with polymyxin B being the most commonly used today due to its efficacy and lower nephrotoxicity compared to polymyxin A.
Mechanism of Action
The mechanism of action of neomycin and polymyxin differs, which explains their synergistic effect when used together. Neomycin works by binding to the bacterial 30S ribosomal subunit, interfering with protein synthesis, which is essential for bacterial growth and replication. This interference leads to the misreading of mRNA, resulting in the synthesis of abnormal proteins that are non-functional, ultimately causing bacterial cell death.
Polymyxin B, on the other hand, acts by interacting with the bacterial cell membrane. It binds to the lipopolysaccharide (LPS) component of the outer membrane of Gram-negative bacteria, disrupting the membrane structure. This disruption leads to the loss of cellular contents and eventually to the death of the bacterial cell. The combination of neomycin and polymyxin B provides a two-pronged attack on bacterial cells, making it difficult for bacteria to develop resistance.
Clinical Uses and Applications
The neomycin and polymyxin B combination is used in various clinical settings, primarily for the treatment of external infections where the risk of systemic absorption is minimal. Common applications include:
- Ophthalmic Infections: For the treatment of conjunctivitis and other superficial infections of the eye.
- Otitis Externa: To treat infections of the external ear canal.
- Skin Infections: For minor skin infections, including those caused by bacteria susceptible to neomycin and polymyxin B.
Safety and Side Effects
While the neomycin and polymyxin combination is generally safe when used topically or externally, there are potential side effects and considerations, especially with prolonged use or in sensitive individuals. These may include:
- Allergic Reactions: Some individuals may develop an allergic reaction to one or both of the antibiotics, manifesting as itching, redness, or swelling at the application site.
- Ototoxicity and Nephrotoxicity: Although less common with topical use, the potential for ototoxicity (damage to the ear) and nephrotoxicity (kidney damage) exists, particularly if the drugs are absorbed systemically in significant quantities.
- Superinfections: As with any antibiotic, there is a risk of superinfection, where the use of the antibiotic leads to an overgrowth of non-susceptible organisms, such as fungi.
Comparative Analysis with Other Antibiotics
The choice of neomycin and polymyxin B over other antibiotics depends on several factors, including the type of infection, the suspected or identified causative bacteria, and the potential for resistance. This combination offers broad-spectrum coverage and is particularly useful against infections caused by Gram-negative bacteria, such as Pseudomonas aeruginosa, which can be challenging to treat. However, it may not be as effective against certain Gram-positive bacteria or fungal infections, necessitating the use of other specific antibiotics or antifungal agents.
Future Trends and Developments
The ongoing challenge of antibiotic resistance necessitates continuous research into new antibiotics and combination therapies. While neomycin and polymyxin B remain effective against a range of bacterial infections, there is a growing need for novel agents that can combat resistant strains. This includes not only the development of new chemical entities but also the exploration of alternative approaches, such as bacteriophage therapy and antimicrobial peptides.
Conclusion
The combination of neomycin and polymyxin B represents a valuable therapeutic option for the treatment of various bacterial infections. Its broad-spectrum activity and efficacy against Gram-negative bacteria make it a preferred choice for several clinical applications. However, it is crucial to use these antibiotics judiciously, considering the potential for side effects and the ever-present threat of antibiotic resistance. As we move forward, the development of new antimicrobial agents and strategies will be essential to staying ahead of emerging resistant bacterial strains.
What is the primary mechanism of action of neomycin?
+Neomycin works by binding to the bacterial 30S ribosomal subunit, interfering with protein synthesis, which is essential for bacterial growth and replication.
How does polymyxin B interact with bacterial cells?
+Polymyxin B interacts with the bacterial cell membrane by binding to the lipopolysaccharide (LPS) component of the outer membrane of Gram-negative bacteria, disrupting the membrane structure and leading to the death of the bacterial cell.
What are common applications of the neomycin and polymyxin B combination?
+Common applications include the treatment of ophthalmic infections, otitis externa, and minor skin infections caused by susceptible bacteria.
What are potential side effects of using neomycin and polymyxin B?
+Potential side effects include allergic reactions, ototoxicity, nephrotoxicity, and the risk of superinfections. However, these are generally minimized with topical use.
Why is the development of new antibiotics important?
+The development of new antibiotics is crucial due to the ongoing challenge of antibiotic resistance. As bacteria evolve resistance to existing antibiotics, new agents are needed to effectively treat infections and prevent the spread of resistant strains.