Pulmonary Embolism Embolism
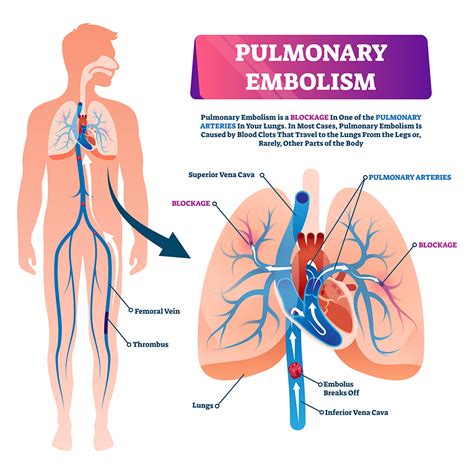
Pulmonary embolism is a potentially life-threatening condition that occurs when a blood clot, known as an embolus, breaks loose from its site of formation and travels through the bloodstream to lodge in one of the pulmonary arteries, which supply blood to the lungs. This blockage can severely impair the lung’s ability to oxygenate blood, leading to a range of symptoms and complications, some of which can be fatal if not promptly and appropriately treated.
Understanding the pathophysiology of pulmonary embolism is crucial for both prevention and treatment. The condition often originates from deep vein thrombosis (DVT), where a clot forms in the deep veins of the legs or other areas of the body. Parts of this clot can break off, becoming emboli that travel through the bloodstream. When these emboli reach the lungs, they can block one or more pulmonary arteries, leading to a pulmonary embolism.
Symptoms of pulmonary embolism can vary widely among individuals but often include sudden onset of shortness of breath, chest pain that worsens with deep breathing, and cough, which may produce bloody sputum. Other symptoms can include rapid heart rate, sweating, and a feeling of anxiety or fainting. In severe cases, pulmonary embolism can lead to collapse, shock, and even death.
Risk Factors and Prevention
Several factors increase an individual’s risk of developing pulmonary embolism. These include a history of DVT or pulmonary embolism, prolonged periods of immobility (such as during long flights or bed rest), surgery, especially on the hips or knees, cancer, and genetic conditions that affect blood clotting, such as factor V Leiden. Pregnancy, older age, and being overweight also contribute to an increased risk.
Prevention strategies focus on reducing the risk of forming blood clots. For individuals at high risk, such as those undergoing major surgery, anticoagulant medications may be prescribed to prevent clot formation. Mobilization, as soon as possible after surgery or during periods of prolonged immobility, and the use of compression stockings can also help prevent DVT and, by extension, pulmonary embolism.
Diagnosis and Treatment
Diagnosing pulmonary embolism typically involves a combination of clinical evaluation, imaging tests, and laboratory assessments. A chest X-ray, electrocardiogram (ECG), and blood tests, including D-dimer levels, are common initial steps. However, computed tomography pulmonary angiography (CTPA) is the preferred imaging test for confirming the diagnosis, as it provides direct visualization of the pulmonary arteries and any emboli.
Treatment of pulmonary embolism is primarily aimed at preventing further clot formation and, if possible, dissolving existing clots. Anticoagulant medications are the cornerstone of treatment for most patients. In severe cases, where the patient’s life is at risk, thrombolytic therapy may be used to dissolve the clot. This approach carries a higher risk of bleeding complications and is typically reserved for life-threatening situations.
Advanced Therapies and Management
For patients with large pulmonary emboli or those who are hemodynamically unstable, more aggressive treatments may be necessary. Catheter-directed thrombolysis involves delivering clot-dissolving medication directly to the clot via a catheter. Surgical embolectomy, where the clot is surgically removed, is another option, although it is associated with significant risks and is generally considered a last resort.
In addition to these acute treatments, management of pulmonary embolism involves addressing underlying risk factors and conditions to prevent recurrence. This may include long-term anticoagulation therapy, lifestyle modifications, and close monitoring for signs of further clotting or embolic events.
Prognosis and Quality of Life
The prognosis for patients with pulmonary embolism varies widely depending on the severity of the condition, promptness and effectiveness of treatment, and the presence of underlying health conditions. For many patients, especially those with smaller, more peripheral clots, treatment can lead to a full recovery. However, some patients may experience chronic complications, such as pulmonary hypertension, which can significantly impact quality of life.
In conclusion, pulmonary embolism is a serious condition that requires immediate medical attention. Understanding its causes, recognizing its symptoms, and implementing preventive measures are crucial steps in managing this potentially life-threatening condition. Advancements in diagnostic techniques and treatment options continue to improve outcomes for patients with pulmonary embolism, emphasizing the importance of ongoing research and clinical vigilance.
What are the common symptoms of pulmonary embolism?
+The symptoms of pulmonary embolism can vary but often include sudden onset of shortness of breath, chest pain that worsens with deep breathing, cough, rapid heart rate, and sweating. In severe cases, it can lead to collapse, shock, and even death.
How is pulmonary embolism diagnosed?
+Diagnosis typically involves a combination of clinical evaluation, imaging tests like computed tomography pulmonary angiography (CTPA), and laboratory assessments, including blood tests for D-dimer levels.
What are the treatment options for pulmonary embolism?
+Treatment primarily involves anticoagulant medications to prevent further clot formation. In severe cases, thrombolytic therapy to dissolve the clot or surgical removal of the clot may be necessary.