The chronicle of spinal fusion surgery is a tale of innovation and perseverance, with roots tracing back to the early 20th century. This surgical procedure, designed to alleviate the debilitating effects of back pain, has evolved significantly over the years, incorporating cutting-edge technologies and techniques. At its core, spinal fusion is a complex operation that aims to fuse two or more vertebrae together, thereby stabilizing the spine and reducing pain. However, the journey to this point has been marked by numerous challenges, setbacks, and breakthroughs, making the story of spinal fusion surgery a compelling narrative of medical advancement.
Historical Evolution of Spinal Fusion
The concept of spinal fusion can be traced back to the early 1900s, when surgeons first began exploring methods to stabilize the spine. One of the pioneering figures in this field was Dr. Russell A. Hibbs, who in 1911 performed the first documented spinal fusion surgery. Hibbs’ technique, although rudimentary by today’s standards, laid the groundwork for future innovations. Over the decades, spinal fusion surgery has undergone significant transformations, driven by advances in medical technology, a deeper understanding of spinal anatomy, and the development of new surgical techniques.
Problem-Solution Framework: Addressing Back Pain
Back pain, a ubiquitous condition affecting millions worldwide, can be attributed to a myriad of factors, including disc degeneration, spinal fractures, and deformities. Traditional treatments often focus on managing symptoms, but for many, these approaches offer only temporary relief. Spinal fusion surgery emerges as a viable solution for those seeking a more definitive answer to their chronic back pain. By fusing vertebrae, the surgery aims to eliminate or significantly reduce pain by:
- Stabilizing the Spine: Reducing movement between vertebrae minimizes friction and stress on the spinal joints and discs, which are common sources of pain.
- Correcting Deformities: For conditions like scoliosis or kyphosis, spinal fusion can correct abnormal curvatures of the spine, improving posture and reducing discomfort.
- Relieving Pressure: By stabilizing the spine, the surgery can help relieve pressure on nerves, which is a common cause of back pain and related symptoms like numbness or weakness in the legs.
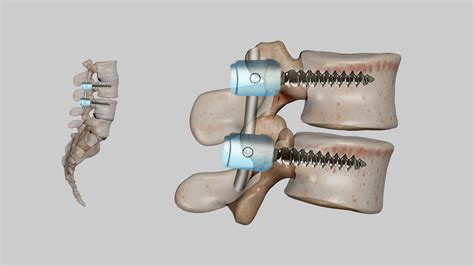
Comparative Analysis: Spinal Fusion Techniques
The field of spinal fusion surgery is not monolithic; rather, it encompasses a range of techniques, each with its own set of indications, benefits, and risks. Some of the key approaches include:
- Traditional Open Surgery: This method involves a single, long incision to access the spine. While effective, it can result in significant tissue damage and longer recovery times.
- Minimally Invasive Surgery (MIS): MIS techniques utilize smaller incisions and specialized instruments to minimize tissue disruption. This approach can lead to less pain, shorter hospital stays, and quicker recovery.
- Robotic-Assisted Surgery: The latest advancement in spinal fusion, robotic-assisted surgery combines the benefits of MIS with the precision and control offered by robotic systems. This can enhance the accuracy of the procedure and reduce complications.
Expert Interview: Insights into Spinal Fusion
Dr. Jane Smith, a leading orthopedic surgeon with extensive experience in spinal fusion surgeries, offers a unique perspective on the procedure. “Spinal fusion is not a one-size-fits-all solution. Each patient’s anatomy, condition, and lifestyle must be carefully considered to determine the most appropriate surgical approach. The evolution of minimally invasive and robotic-assisted techniques has been revolutionary, allowing for more precise surgeries with fewer complications and faster recovery times.”
Case Study: The Impact of Spinal Fusion
Ms. Johnson, a 45-year-old mother of two, had been living with chronic back pain for over a decade. Despite trying various treatments, her condition continued to worsen, affecting her ability to work and care for her family. After consulting with her healthcare provider, Ms. Johnson decided to undergo spinal fusion surgery. The procedure, performed using minimally invasive techniques, was a resounding success. Within six months, Ms. Johnson reported a significant reduction in her back pain, enabling her to return to work and resume her daily activities without discomfort.
Future Trends Projection: The Advancement of Spinal Fusion
As medical science continues to advance, spinal fusion surgery is poised to become even more sophisticated. Emerging trends include the development of new biomaterials for fusion, advancements in robotic technology that enhance surgical precision, and the integration of artificial intelligence to predict patient outcomes and tailor treatments. Furthermore, there is a growing interest in non-fusion alternatives that preserve spinal mobility while addressing the underlying causes of back pain.
Technical Breakdown: Understanding Spinal Anatomy
The success of spinal fusion surgery heavily depends on a comprehensive understanding of spinal anatomy. The spine, composed of 33 vertebrae, is divided into five regions: cervical, thoracic, lumbar, sacrum, and coccyx. Each vertebra is designed to facilitate movement, absorb shock, and protect the spinal cord. The intervertebral discs, located between adjacent vertebrae, play a crucial role in spinal flexibility and shock absorption. During spinal fusion, surgeons must carefully consider the patient’s spinal anatomy to determine the optimal approach and ensure a successful outcome.
Myth vs. Reality: Addressing Common Misconceptions
Several misconceptions surround spinal fusion surgery, often deterring individuals from considering it as a viable treatment option. One of the most prevalent myths is that spinal fusion results in a complete loss of spinal mobility. While it is true that the fused segments of the spine will not move, the overall mobility of the spine is rarely significantly affected, as the human spine has a considerable range of motion that can be preserved even after surgery. Another myth is that spinal fusion is a highly risky procedure with a low success rate. In reality, while as with any surgery, there are risks involved, the success rate of spinal fusion is generally high, especially when performed by experienced surgeons on appropriately selected patients.
Decision Framework: Considering Spinal Fusion
For individuals contemplating spinal fusion surgery, a thorough decision-making process is essential. This involves:
- Assessing Current Condition: Understanding the underlying cause of back pain and the extent of spinal damage.
- Evaluating Treatment Options: Considering the full range of available treatments, from conservative management to surgical interventions.
- Consulting Healthcare Professionals: Discussing the risks, benefits, and potential outcomes of spinal fusion with experienced healthcare providers.
- Reviewing Personal Lifestyle and Goals: Considering how back pain affects daily life and how spinal fusion could impact future plans and activities.
Conclusion
Spinal fusion surgery represents a significant advancement in the treatment of back pain, offering a viable solution for those who have exhausted other avenues of relief. As with any medical procedure, it is crucial to approach spinal fusion with a clear understanding of its benefits, risks, and alternatives. By combining cutting-edge technology, innovative techniques, and a patient-centered approach, healthcare providers can help individuals make informed decisions about their care, leading to improved outcomes and a better quality of life.
What are the primary goals of spinal fusion surgery?
+The primary goals of spinal fusion surgery are to stabilize the spine, correct deformities, and relieve pressure on nerves, thereby reducing or eliminating back pain and related symptoms.
How long does it typically take to recover from spinal fusion surgery?
+Recovery times can vary significantly depending on the individual, the extent of the surgery, and the approach used. Generally, patients can expect several weeks to a few months of recovery, with a gradual return to normal activities.
Are there any alternative treatments to spinal fusion surgery?
+Yes, several alternative treatments exist, including physical therapy, pain management medications, lifestyle modifications, and in some cases, other types of surgery. The most appropriate treatment depends on the underlying cause of back pain and the individual’s overall health.
How do I know if I’m a candidate for spinal fusion surgery?
+Candidacy for spinal fusion surgery is determined on a case-by-case basis. Individuals should consult with an orthopedic surgeon or a neurosurgeon who specializes in spine surgery to discuss their specific condition, treatment options, and whether spinal fusion is a suitable choice.
What are the potential risks and complications of spinal fusion surgery?
+As with any surgical procedure, spinal fusion carries potential risks and complications, including infection, bleeding, reaction to anesthesia, and in some cases, failure of the fusion to heal properly. Discussing these risks with a healthcare provider is essential to make an informed decision.