Testing Breast Cancer Gene
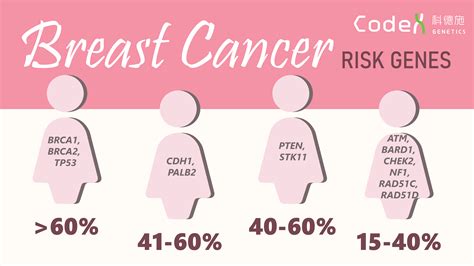
Breast cancer is a complex and multifaceted disease that affects millions of people worldwide. One of the most significant advances in understanding and combating breast cancer has been the discovery of genetic mutations that contribute to its development. Among these, the BRCA1 and BRCA2 genes are the most well-known, but there are other genes that also play critical roles. Testing for these genetic mutations has become an essential tool in the prevention, diagnosis, and treatment of breast cancer.
Understanding BRCA1 and BRCA2
The BRCA1 and BRCA2 genes are tumor suppressor genes, which means they help repair damaged DNA and thus play a crucial role in ensuring the stability of a cell’s genetic material. When either of these genes is mutated, or altered, such that its function is impaired, DNA damage may not be properly repaired. This can lead to more genetic alterations that can result in cancer. Women with a mutation in one of these genes have a significantly increased risk of developing breast and ovarian cancer, among other cancers.
The Process of Genetic Testing
Genetic testing for breast cancer involves a blood test or, less commonly, a saliva test, that looks for mutations in the BRCA1 and BRCA2 genes, as well as other genes that may increase the risk of breast cancer. The process begins with a consultation with a genetic counselor or other healthcare provider to discuss the appropriateness of testing, based on family history, personal medical history, and other factors. If the decision is made to proceed with testing, a sample is sent to a laboratory for analysis.
Who Should Consider Genetic Testing?
Not everyone needs to undergo genetic testing for breast cancer. The decision to have genetic testing is based on several factors, including:
- Family History: A history of breast, ovarian, or other related cancers in close relatives, especially if these cancers occurred at a younger age.
- Personal Medical History: A personal history of breast cancer, especially if diagnosed at a young age.
- Ethnic Background: Certain ethnic groups, such as Ashkenazi Jewish individuals, have a higher prevalence of BRCA1 and BRCA2 mutations.
Interpreting Test Results
The results of genetic testing can be complex and require careful interpretation by a healthcare provider or genetic counselor. Results can indicate:
- Positive Result: A mutation associated with an increased risk of breast cancer is found. This does not mean that the individual will definitely develop breast cancer, but rather that their risk is higher than average.
- Negative Result: No mutation is found in the genes tested. However, this does not guarantee that the individual will not develop breast cancer, as many cases are not associated with known genetic mutations.
- Variant of Uncertain Significance (VUS): A change in the gene is found, but it is not known whether this change affects the risk of cancer. Further research and testing may be needed.
What to Do with the Results
Individuals who test positive for a mutation associated with an increased risk of breast cancer have several options to consider:
- Enhanced Screening: More frequent and/or advanced screening methods, such as annual MRI in addition to mammography.
- Risk-Reducing Surgery: Surgical removal of the breasts (prophylactic mastectomy) and/or ovaries (prophylactic salpingo-oophorectomy) to reduce the risk of developing cancer in these organs.
- Chemoprevention: The use of medications to reduce the risk of breast cancer.
Each of these options carries its own set of considerations, including potential benefits, risks, and emotional impacts. Decisions are highly personal and should be made in consultation with healthcare providers.
Emerging Advances in Genetic Testing
The field of genetic testing for breast cancer is rapidly evolving. Next-generation sequencing (NGS) technologies allow for the simultaneous analysis of multiple genes, providing a more comprehensive assessment of cancer risk. Additionally, research into other genetic mutations and their roles in breast cancer is ongoing, which may lead to more targeted and effective strategies for prevention and treatment.
Conclusion
Genetic testing for breast cancer represents a powerful tool in the fight against this disease. By understanding an individual’s genetic predisposition, tailored strategies for screening, prevention, and treatment can be developed. While genetic testing is not a guarantee against developing breast cancer, it provides valuable information that can help individuals and their healthcare providers make informed decisions about their health.
Frequently Asked Questions
What does it mean to have a BRCA1 or BRCA2 gene mutation?
+Having a mutation in one of these genes means you have a higher risk of developing breast and ovarian cancer. However, it's important to note that not everyone with a mutation will develop cancer, and many breast cancers occur in individuals without these mutations.
How accurate is genetic testing for breast cancer?
+Genetic testing for breast cancer is highly accurate for detecting known mutations in genes like BRCA1 and BRCA2. However, no test can detect all possible genetic mutations, and the interpretation of results can be complex, requiring consultation with a genetic counselor or healthcare provider.
Can genetic testing predict the exact risk of developing breast cancer?
+While genetic testing can provide information about increased risk, it cannot predict with certainty who will develop breast cancer. Many factors, including lifestyle, environment, and other genetic factors, contribute to an individual's overall risk.
As research continues to advance, the role of genetic testing in breast cancer will likely expand, offering more precise and personalized approaches to health management. For now, it remains a critical component of breast cancer prevention and treatment strategies, empowering individuals with knowledge to make informed decisions about their health.