Type 2 Diabetes Glucose Levels
Managing type 2 diabetes requires a deep understanding of how glucose levels fluctuate throughout the day and how different factors can influence these levels. At the core of diabetes management is the concept of glucose control, which involves maintaining blood glucose levels within a target range to prevent complications and improve quality of life.
Understanding Glucose Levels
Glucose is a type of sugar that serves as the body’s primary source of energy. In individuals with type 2 diabetes, the body either resists the effects of insulin, a hormone produced by the pancreas that regulates blood sugar levels, or doesn’t produce enough insulin to maintain a normal glucose level. As a result, glucose builds up in the bloodstream, leading to high blood sugar levels.
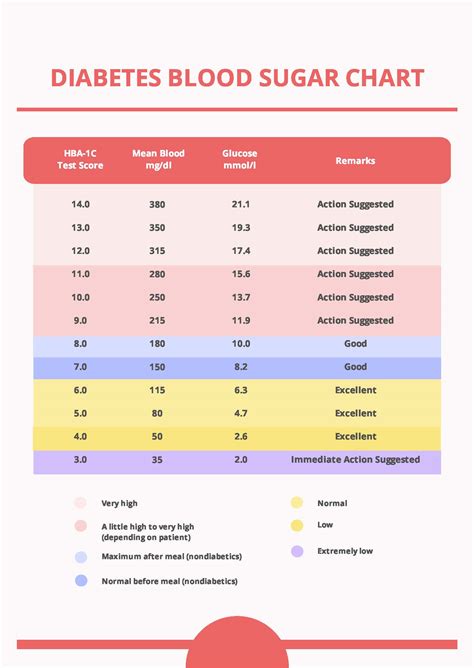
Normal blood glucose levels typically range from 70 to 99 mg/dL when fasting and are less than 140 mg/dL after meals. For individuals with diabetes, the American Diabetes Association recommends the following target glucose levels:
- Fasting glucose levels: Less than 130 mg/dL
- Before meals: 70 to 130 mg/dL
- After meals (1-2 hours): Less than 180 mg/dL
Factors Affecting Glucose Levels
Several factors can cause blood glucose levels to fluctuate, including:
- Diet: Consuming high-carbohydrate foods, especially those with a high glycemic index, can cause blood glucose levels to spike.
- Physical Activity: Regular physical activity can lower blood glucose levels and improve insulin sensitivity.
- Medications: Certain medications, including those for diabetes, can affect glucose levels.
- Stress: Stress can raise blood glucose levels by stimulating the release of stress hormones like cortisol and adrenaline.
- Sleep: Lack of quality sleep or having sleep disorders can affect glucose metabolism and insulin sensitivity.
- Illness: Being sick can cause blood glucose levels to rise due to the body’s stress response.
- Hormonal Changes: Hormonal fluctuations during menstruation, pregnancy, or menopause can impact glucose levels.
Monitoring and Managing Glucose Levels
Effective management of type 2 diabetes involves regular monitoring of blood glucose levels, a balanced diet, regular physical activity, and, if prescribed, medication. Here are some strategies for managing glucose levels:
- Blood Glucose Monitoring: Regularly checking blood glucose levels helps individuals with diabetes understand how different factors affect their glucose levels and make informed decisions about their care.
- Meal Planning: Eating a balanced diet that is low in added sugars, saturated fats, and sodium, and high in fiber can help manage blood glucose levels. Considering the glycemic index of foods can also be helpful.
- Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or an equivalent combination of both, per week, can improve insulin sensitivity and lower glucose levels.
- Medication Adherence: If medication is part of the treatment plan, taking it as directed is crucial for maintaining target glucose levels.
Complications of Unmanaged Glucose Levels
Unmanaged or poorly managed diabetes can lead to serious complications, including:
- Heart Disease and Stroke: High blood glucose levels can damage blood vessels and the nerves that control the heart.
- Kidney Damage: Diabetes is the leading cause of chronic kidney disease and kidney failure.
- Nerve Damage: High blood glucose can damage the nerves, leading to pain, numbness, and weakness in the hands and feet.
- Eye Damage: Diabetes can cause blindness if left unmanaged by damaging the blood vessels in the retina.
- Foot Damage: Nerve damage and poor circulation can lead to foot ulcers and, in severe cases, amputation.
Conclusion
Managing type 2 diabetes is a multifaceted approach that involves monitoring and controlling glucose levels, adopting a healthy lifestyle, and, when necessary, using medication. By understanding the factors that influence glucose levels and implementing effective management strategies, individuals with type 2 diabetes can reduce their risk of complications and improve their overall quality of life.
What are normal glucose levels for someone without diabetes?
+For individuals without diabetes, normal blood glucose levels are typically between 70 to 99 mg/dL when fasting and less than 140 mg/dL after meals.
How does diet affect glucose levels in type 2 diabetes?
+Diet plays a crucial role in managing type 2 diabetes. Consuming foods that are low on the glycemic index, rich in fiber, and low in added sugars and saturated fats can help manage blood glucose levels. It's also important to be mindful of portion sizes to avoid consuming too many carbohydrates at once.
What are the potential complications of unmanaged type 2 diabetes?
+Unmanaged or poorly managed type 2 diabetes can lead to serious complications, including heart disease, stroke, kidney damage, nerve damage, eye damage, and foot damage. Maintaining good glucose control through diet, exercise, and medication (if prescribed) is key to preventing these complications.
By focusing on the management of glucose levels and adopting a comprehensive approach to health, individuals with type 2 diabetes can lead active, healthy lives and reduce the risk of long-term complications.