When Does Chest Pain Indicate Musculoskeletal Issues? Diagnostic Tips
Chest pain is a symptom that often prompts immediate concern, and rightly so, given its potential association with serious cardiac conditions. However, not all chest pain is related to the heart. Musculoskeletal issues, which affect the muscles, bones, and joints, can also cause chest pain, sometimes mimicking the symptoms of more severe conditions. Distinguishing between cardiac and musculoskeletal causes of chest pain is crucial for appropriate diagnosis and treatment. This article will delve into when chest pain might indicate musculoskeletal issues, providing diagnostic tips for healthcare professionals and insights for individuals experiencing such symptoms.
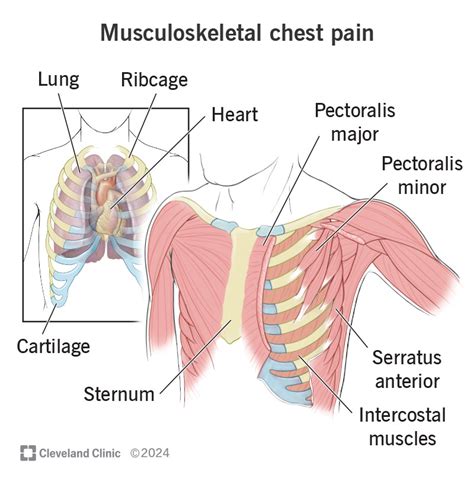
Understanding Musculoskeletal Chest Pain
Musculoskeletal chest pain originates from the structures that make up the chest wall, including the muscles, bones, and cartilage. This type of pain can be acute or chronic and is often related to trauma, overuse, or inflammatory conditions. Common musculoskeletal sources of chest pain include costochondritis (inflammation of the cartilage that connects the ribs to the breastbone), Tietze’s syndrome (a condition similar to costochondritis but can involve the surrounding muscles), and muscle strain.
Clinical Presentation
Musculoskeletal chest pain typically presents with certain characteristics that can help differentiate it from cardiac causes:
- Location and Radiation: The pain is often localized to the chest wall and can be reproduced by palpation or movement of the affected area. It may radiate to the arms, but this is less common than in cardiac conditions.
- Quality and Intensity: Described as sharp, stabbing, or aching, the pain can range from mild to severe. Its intensity may increase with movement or deep breathing.
- Triggering Factors: Activities that involve heavy lifting, bending, or repetitive movements can trigger or exacerbate the pain.
- Associated Symptoms: While there might be some overlap, musculoskeletal pain is less likely to be associated with symptoms like dyspnea (difficulty breathing), diaphoresis (sweating), or nausea, which are more commonly seen in cardiac conditions.
Diagnostic Approach
Diagnosing musculoskeletal chest pain involves a combination of clinical evaluation, physical examination, and sometimes, diagnostic imaging:
- History Taking: A detailed history can help identify potential causes, such as recent trauma, changes in activity level, or previous musculoskeletal conditions.
- Physical Examination: Palpation of the chest wall to identify tender points, and maneuvers that reproduce the pain, such as movement of the arms or deep breathing, can be diagnostic.
- Imaging Studies: While not always necessary, X-rays, ultrasound, or MRI can be used to rule out other causes of chest pain or to confirm musculoskeletal pathology, such as fractures or muscle tears.
Diagnostic Tips
- Consider the Patient’s Profile: Younger individuals with no cardiac risk factors and a history suggestive of musculoskeletal trauma or overuse are more likely to have a musculoskeletal cause of their chest pain.
- Look for Localized Tender Points: The presence of tender points on the chest wall that reproduce the patient’s pain upon palpation is highly suggestive of a musculoskeletal origin.
- Utilize the “Special Tests”: Specific maneuvers, such as the “costochondral maneuver” (applying pressure over the costochondral junctions), can help confirm musculoskeletal chest pain.
- Rule Out Red Flags: Always consider and rule out conditions that could mimic musculoskeletal pain but require urgent attention, such as pulmonary embolism or myocardial infarction.
Management and Treatment
The management of musculoskeletal chest pain typically involves conservative measures aimed at relieving pain and reducing inflammation:
- Pain Relief Medications: NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are commonly used to manage pain and inflammation.
- Physical Therapy: Stretching and strengthening exercises can help improve range of motion and reduce strain on the affected muscles.
- Modifying Activities: Avoiding activities that exacerbate the pain and incorporating regular breaks to stretch and move can be beneficial.
Conclusion
Musculoskeletal issues are a common cause of chest pain, distinct from cardiac conditions. A thorough clinical evaluation, including a detailed history and physical examination, is crucial for an accurate diagnosis. Healthcare professionals should be adept at recognizing the characteristics of musculoskeletal chest pain and employ a diagnostic approach that considers the patient’s overall clinical picture. By doing so, appropriate treatment can be initiated, alleviating symptoms and improving quality of life for those affected.
What are the most common musculoskeletal causes of chest pain?
+The most common musculoskeletal causes of chest pain include costochondritis, Tietze’s syndrome, and muscle strain. These conditions affect the chest wall, including the muscles, bones, and cartilage, leading to pain that can sometimes be confused with cardiac issues.
How can musculoskeletal chest pain be differentiated from cardiac chest pain?
+Musculoskeletal chest pain can often be differentiated from cardiac chest pain through its characteristics, such as being localized to the chest wall, reproducible by palpation, and worsening with movement or deep breathing. Additionally, the absence of symptoms like dyspnea, diaphoresis, or nausea can help in distinguishing it from cardiac causes.
What is the typical treatment approach for musculoskeletal chest pain?
+The treatment for musculoskeletal chest pain usually involves conservative measures, including pain relief medications like NSAIDs, physical therapy to improve range of motion and strength, and modifying activities to avoid exacerbating the pain. In some cases, further interventions may be necessary, depending on the underlying cause and severity of the condition.