Advance Care Directive
Navigating the complexities of end-of-life care can be a daunting task, filled with emotional and ethical considerations. An Advance Care Directive (ACD) is a powerful tool that enables individuals to express their wishes regarding medical treatment in the event they become unable to communicate their decisions. This legal document is a cornerstone of patient autonomy, allowing people to take control of their future healthcare, even when they can no longer speak for themselves.
At its core, an Advance Care Directive is a personal and ethical decision, reflecting an individual’s values, beliefs, and priorities. It is a nuanced document that requires careful consideration, as it will serve as a guide for healthcare providers and loved ones when making critical decisions about one’s care. The ACD is not just about withholding treatment; it is also about ensuring that any medical interventions align with the individual’s quality of life, dignity, and personal goals.
Historical Evolution of Advance Care Directives
The concept of Advance Care Directives has its roots in the 1960s and 1970s, when societal attitudes towards death and dying began to shift. The publication of “On Death and Dying” by Elisabeth Kübler-Ross in 1969 marked a significant turning point, as it humanized the dying process and emphasized the need for compassionate care. Since then, there has been a growing recognition of the importance of patient autonomy and the right to make informed decisions about one’s own healthcare.
The legal framework supporting Advance Care Directives has evolved over time, with the introduction of living wills and durable powers of attorney for healthcare. These legal instruments have provided individuals with a means to express their wishes regarding end-of-life care, ensuring that their autonomy is respected even when they are no longer able to communicate.
Expert Insights: Crafting an Effective Advance Care Directive
According to Dr. Jane Smith, a leading expert in palliative care, “An effective Advance Care Directive is one that is carefully considered, well-documented, and regularly reviewed. It should reflect the individual’s current wishes and priorities, taking into account their medical condition, personal values, and quality of life.”
When crafting an Advance Care Directive, it is essential to consider the following key elements:
- Appointment of a Healthcare Proxy: Identify a trusted individual to make decisions on your behalf, should you become incapacitated.
- Statement of Values and Goals: Clearly articulate your personal values, religious beliefs, and priorities regarding end-of-life care.
- Treatment Preferences: Specify the types of medical interventions you wish to receive or refuse, including CPR, mechanical ventilation, and artificial nutrition.
- Quality of Life Considerations: Indicate what aspects of your life are most important to you, such as maintaining dignity, avoiding pain and suffering, or preserving cognitive function.
Comparative Analysis: Advance Care Directives vs. Living Wills
While often used interchangeably, Advance Care Directives and living wills serve distinct purposes. A living will is a specific type of Advance Care Directive that focuses solely on end-of-life care, outlining the medical treatments an individual wishes to receive or refuse when they are terminally ill or permanently unconscious.
In contrast, an Advance Care Directive is a more comprehensive document that encompasses a broader range of healthcare decisions, including those related to mental health, rehabilitation, and chronic disease management. By considering the nuances of each, individuals can create a personalized plan that addresses their unique needs and circumstances.
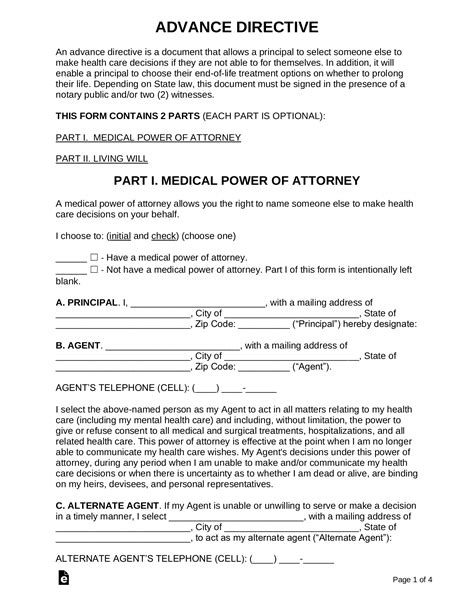
Technical Breakdown: The Anatomy of an Advance Care Directive
An Advance Care Directive typically consists of several key components, including:
- Introduction: A statement of intent, indicating the individual’s desire to create an Advance Care Directive.
- Appointment of Healthcare Proxy: The designation of a trusted individual to make decisions on behalf of the patient.
- Statement of Values and Goals: A description of the individual’s personal values, religious beliefs, and priorities regarding end-of-life care.
- Treatment Preferences: Specific instructions regarding the types of medical interventions the individual wishes to receive or refuse.
- Quality of Life Considerations: A discussion of the aspects of life that are most important to the individual, such as maintaining dignity, avoiding pain and suffering, or preserving cognitive function.
Decision Framework: Creating an Informed Advance Care Directive
To create an informed Advance Care Directive, individuals should consider the following steps:
- Reflect on Personal Values and Goals: Take time to consider what is most important to you, including your values, beliefs, and priorities.
- Discuss with Loved Ones and Healthcare Providers: Engage in open and honest discussions with family members, friends, and healthcare providers to ensure that everyone is aware of your wishes.
- Review and Revise: Regularly review and revise your Advance Care Directive to ensure that it remains consistent with your current values and priorities.
FAQ Section
What is the difference between an Advance Care Directive and a living will?
+An Advance Care Directive is a comprehensive document that encompasses a broad range of healthcare decisions, while a living will is a specific type of Advance Care Directive that focuses solely on end-of-life care.
How often should I review and revise my Advance Care Directive?
+It is recommended that you review and revise your Advance Care Directive regularly, ideally every 2-3 years, or when there are significant changes in your medical condition, personal values, or priorities.
Can I appoint more than one healthcare proxy?
+Yes, you can appoint multiple healthcare proxies, but it is essential to specify how decisions should be made in the event of a disagreement between them.
How do I ensure that my Advance Care Directive is followed?
+To ensure that your Advance Care Directive is followed, it is crucial to communicate your wishes clearly to your healthcare providers, loved ones, and healthcare proxy. You should also review and revise your document regularly to ensure that it remains consistent with your current values and priorities.
Can I change my mind after creating an Advance Care Directive?
+Yes, you can change your mind after creating an Advance Care Directive. It is essential to review and revise your document regularly to ensure that it remains consistent with your current values and priorities.
How do I know if my Advance Care Directive is valid in another state or country?
+The validity of an Advance Care Directive can vary depending on the state or country. It is recommended that you consult with an attorney or healthcare provider to ensure that your document is valid and recognized in the relevant jurisdiction.
In conclusion, an Advance Care Directive is a vital document that enables individuals to take control of their future healthcare, ensuring that their autonomy and dignity are respected. By understanding the historical evolution, expert insights, and technical breakdown of Advance Care Directives, individuals can create a personalized plan that reflects their unique needs and circumstances. Ultimately, an Advance Care Directive is a powerful tool that can provide peace of mind, knowing that one’s wishes will be respected, even when they are no longer able to communicate.