Hepatitis A Ab Reactive
The presence of Hepatitis A antibodies (anti-HAV) in the blood indicates that an individual has been exposed to the Hepatitis A virus (HAV) at some point in their lives. This exposure could have resulted from an active infection, which the person’s immune system was able to clear, or from vaccination against Hepatitis A. The detection of these antibodies, referred to as a “Hepatitis A Ab reactive” result, signifies immunity to the virus, meaning the individual is protected against future infections.
Understanding the Hepatitis A Virus
Hepatitis A is a highly contagious liver infection caused by the Hepatitis A virus. It is primarily spread through the fecal-oral route, where the virus is ingested, usually through contaminated food or water or through direct contact with an infected person. The virus can also be spread through less common routes, such as through blood transfusions, although this is rare in areas with thorough blood screening.
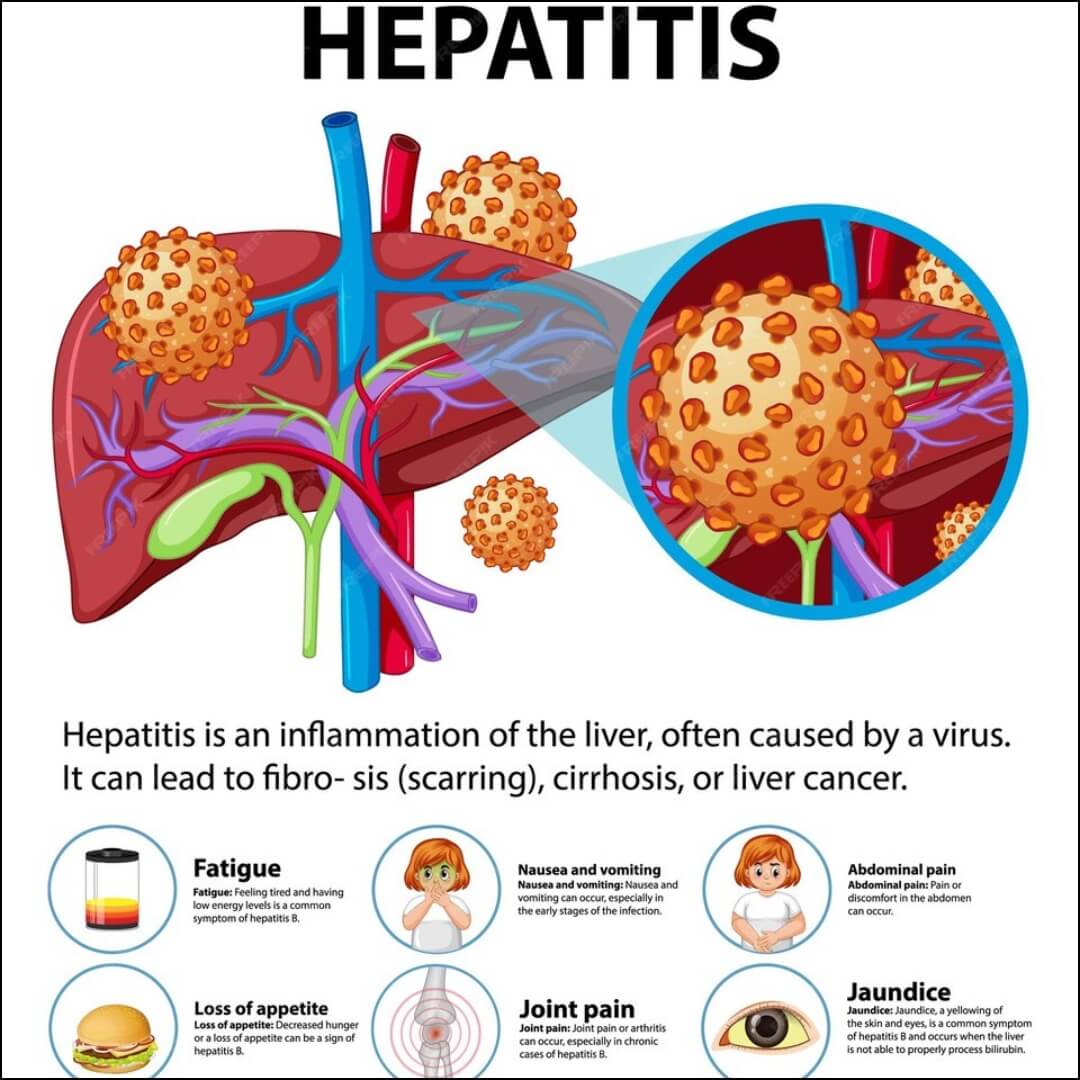
Symptoms of Hepatitis A infection can range from mild to severe and include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, and jaundice (a condition that causes the skin and eyes to turn yellow). However, many individuals, especially children, may not exhibit any symptoms at all.
Interpretation of Hepatitis A Antibody Test Results

IgM Anti-HAV
- Presence of IgM anti-HAV indicates an acute (recent) Hepatitis A infection. This is because IgM antibodies are the first line of defense and are produced in response to an initial infection. They typically appear within the first few weeks after exposure and can remain detectable for up to six months.
IgG Anti-HAV
- Presence of IgG anti-HAV signifies a past infection or vaccination. IgG antibodies are produced later in the course of the infection and provide long-term immunity. They can be detected in the blood months to years after the initial infection has resolved and indicate that the person is no longer contagious.
Clinical Implications and Public Health Considerations
The detection of Hepatitis A antibodies has significant implications for both clinical management and public health policy:
Immunity: Individuals with reactive Hepatitis A antibodies, particularly IgG anti-HAV, are considered immune to the virus. This immunity is lifelong in most cases, protecting against future infections and reducing the risk of transmitting the virus to others.
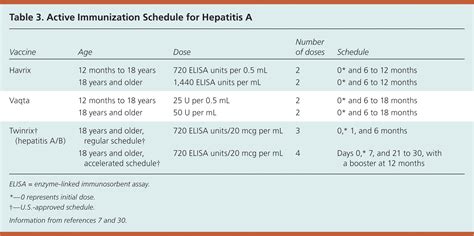
Vaccination: For those who have not been infected or vaccinated, Hepatitis A vaccination is recommended, especially for travelers to areas with high or intermediate prevalence of Hepatitis A, individuals with certain medical conditions, and those whose sexual practices or drug use increases their risk.
Outbreak Control: In the event of a Hepatitis A outbreak, public health measures such as improved sanitation, hygiene practices, and targeted vaccination efforts can help control the spread of the virus.
Screening: Routine screening for Hepatitis A is not typically recommended for the general population but may be advised for individuals at increased risk of infection.
Conclusion
A “Hepatitis A Ab reactive” result indicates the presence of immunity to the Hepatitis A virus, either through past infection or successful vaccination. Understanding the implications of this result is crucial for assessing individual risk, guiding preventive measures, and informing public health strategies to reduce the incidence of Hepatitis A infections.
What does a Hepatitis A Ab reactive result mean?
+A Hepatitis A Ab reactive result means that the individual has Hepatitis A antibodies in their blood, indicating past infection or vaccination and implying immunity to the virus.
How is Hepatitis A typically spread?
+Hepatitis A is primarily spread through the fecal-oral route, involving contaminated food or water, or through direct contact with an infected person.
What are the implications of having IgG anti-HAV antibodies?
+The presence of IgG anti-HAV antibodies indicates past infection or vaccination and signifies long-term immunity to Hepatitis A, protecting against future infections.
In the broader context of liver health and infectious diseases, understanding and addressing Hepatitis A is crucial. As research and medical practices evolve, the approach to diagnosing, treating, and preventing Hepatitis A will continue to improve, relying on the sophisticated interplay between clinical medicine, public health initiatives, and individual awareness and action.