Spinal Fusion Surgery
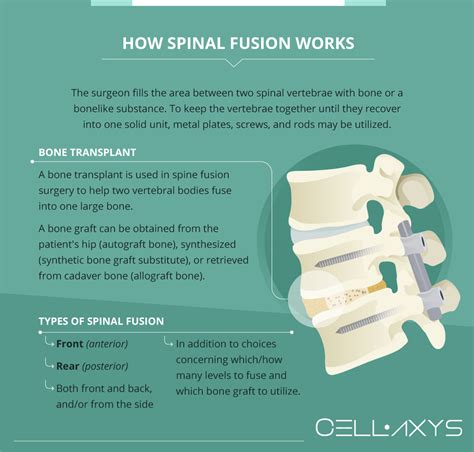
Spinal fusion surgery is a complex and highly specialized medical procedure designed to combine two or more vertebrae in the spine, effectively eliminating movement between them. This surgical technique is often employed to treat a variety of spinal disorders, including degenerative disc disease, spinal fractures, scoliosis, and spinal instability. By fusing the vertebrae together, the surgery aims to alleviate pain, stabilize the spine, and prevent further damage or deformity.
One of the primary indications for spinal fusion surgery is the presence of severe back pain that has not responded to more conservative treatments, such as physical therapy, medication, or injections. Candidates for this surgery often experience chronic pain and may have difficulty performing daily activities due to spinal instability or deformity. The decision to undergo spinal fusion surgery is typically made after a thorough evaluation by an orthopedic surgeon or neurosurgeon, taking into account the patient’s overall health, the severity of their condition, and the potential benefits and risks of the procedure.
Surgical Techniques
Spinal fusion surgery can be performed using various techniques, each with its own advantages and disadvantages. The choice of technique depends on the location and severity of the spinal condition, as well as the patient’s individual needs and preferences. Some of the most common spinal fusion techniques include:
- Posterolateral Fusion (PLF): This technique involves making an incision in the back to access the spine. The surgeon then removes any damaged disc material and inserts a bone graft between the vertebrae to facilitate fusion.
- Anterior Lumbar Interbody Fusion (ALIF): In this approach, the surgeon makes an incision in the abdomen to access the spine from the front. This technique allows for the removal of the damaged disc and the insertion of a bone graft or cage to promote fusion.
- Transforaminal Lumbar Interbody Fusion (TLIF): A combination of the posterior and anterior approaches, TLIF involves making an incision in the back and removing the damaged disc material. A bone graft or cage is then inserted through the foramen (the space through which the nerve roots exit the spinal canal) to facilitate fusion.
- Minimally Invasive Spinal Fusion: This technique involves using smaller incisions and specialized instruments to minimize tissue damage and promote faster recovery. Minimally invasive approaches can be used for various types of spinal fusion surgeries.
Benefits and Risks
While spinal fusion surgery can offer significant relief from pain and improvement in quality of life for many patients, it is not without risks and complications. Some of the potential benefits of spinal fusion include:
- Pain Relief: By stabilizing the spine and eliminating movement between the fused vertebrae, spinal fusion can significantly reduce or eliminate pain.
- Improved Stability: The fusion of vertebrae can help to correct spinal deformities and prevent further instability.
- Enhanced Functionality: By alleviating pain and improving spinal stability, patients may experience an improvement in their ability to perform daily activities.
However, as with any surgical procedure, there are also potential risks and complications to consider, including:
- Infection: As with any surgery, there is a risk of infection with spinal fusion.
- Blood Clots: Patients may be at risk for developing blood clots in the legs or lungs.
- Nerve Damage: There is a risk of nerve damage during the surgery, which could result in numbness, weakness, or paralysis.
- Pseudarthrosis: This is a condition where the bone graft does not properly fuse, leading to ongoing pain and instability.
- Adjacent Segment Disease: After spinal fusion, the segments of the spine adjacent to the fusion site may be subjected to increased stress, potentially leading to degeneration or instability over time.
Recovery and Rehabilitation
The recovery process from spinal fusion surgery can vary significantly depending on the individual patient, the extent of the surgery, and the technique used. Generally, patients can expect to spend several days in the hospital after surgery, during which time they will be monitored for potential complications and managed for pain. Once discharged, patients typically undergo a period of rehabilitation, which may include physical therapy to improve mobility, strength, and flexibility.
It is crucial for patients to follow their surgeon’s instructions carefully during the recovery period to ensure the best possible outcome. This includes avoiding heavy lifting, bending, or twisting, and gradually increasing activity levels as advised. The fusion process itself can take several months to a year or more to complete, during which time patients will need to attend follow-up appointments with their surgeon to monitor the progress of the fusion and address any concerns or complications that may arise.
Emerging Trends and Technologies
The field of spinal surgery is continuously evolving, with advancements in technology and technique offering new possibilities for treating spinal disorders. Some of the emerging trends and technologies in spinal fusion surgery include:
- Robotic-Assisted Surgery: The use of robotic systems in spinal fusion can enhance precision, reduce complications, and potentially lead to faster recovery times.
- Artificial Disc Replacement: For certain patients, artificial disc replacement may offer an alternative to spinal fusion, aiming to preserve spinal motion and reduce the risk of adjacent segment disease.
- Biologics and Biomaterials: Research into new biologic agents and biomaterials is underway to improve the bone grafting process, potentially leading to more efficient and effective fusion.
Conclusion
Spinal fusion surgery is a significant medical intervention that can offer relief from pain and improvement in quality of life for patients with severe spinal disorders. While it carries potential risks and complications, the benefits can be substantial for appropriately selected candidates. As with any major surgical procedure, careful consideration, thorough evaluation, and consultation with a healthcare professional are essential to determine if spinal fusion surgery is the right treatment option. The ongoing advancements in spinal surgery technologies and techniques hold promise for further improving outcomes and expanding treatment options for patients.
What is the primary goal of spinal fusion surgery?
+The primary goal of spinal fusion surgery is to combine two or more vertebrae in the spine, eliminating movement between them to alleviate pain, stabilize the spine, and prevent further damage or deformity.
What are the common indications for spinal fusion surgery?
+Common indications include severe back pain not responsive to conservative treatments, spinal fractures, scoliosis, and spinal instability. Candidates often experience chronic pain and difficulty with daily activities due to spinal disorders.
What are the risks and complications associated with spinal fusion surgery?
+Risks include infection, blood clots, nerve damage, pseudarthrosis (failure of the bone graft to fuse), and adjacent segment disease. It is essential for patients to be aware of these potential complications and discuss them with their surgeon.
How long does it take to recover from spinal fusion surgery?
+Recovery time can vary but typically involves several days in the hospital, followed by a period of rehabilitation that can last several months. The fusion process itself can take from several months to over a year to complete.
What are some emerging trends and technologies in spinal fusion surgery?
+Emerging trends include the use of robotic-assisted surgery, artificial disc replacement, and advancements in biologics and biomaterials to improve bone grafting and fusion outcomes.



