What Causes Pancreatitis
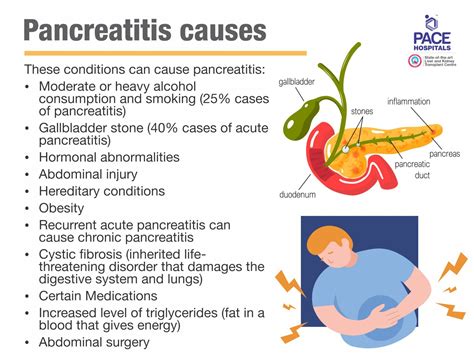
Pancreatitis, a condition characterized by inflammation of the pancreas, can be a debilitating and potentially life-threatening disease. The pancreas, an organ located behind the stomach, plays a vital role in digestion and glucose regulation by producing digestive enzymes and hormones like insulin. Understanding the causes of pancreatitis is crucial for prevention, diagnosis, and treatment.
Gallstones: A Common Cause
Gallstones are solid particles that form in the gallbladder, a small organ located under the liver that stores bile. These stones can sometimes block the pancreatic duct, which is the tube that carries pancreatic juices into the intestine. This blockage can cause inflammation of the pancreas, leading to pancreatitis. The relationship between gallstones and pancreatitis is well-established, with gallstones being one of the most common causes of acute pancreatitis.
Alcohol Consumption
Alcohol consumption is another significant cause of pancreatitis, particularly chronic pancreatitis. Alcohol can cause the pancreatic ducts to become inflamed and can lead to the formation of stones within the pancreas. It is believed that alcohol metabolism produces toxic substances that harm the pancreas. Chronic alcohol consumption can lead to irreversible damage to the pancreas, resulting in chronic pancreatitis, which is characterized by persistent inflammation and scarring of the pancreas.
Genetic Factors
Some people are born with genetic conditions that increase their risk of developing pancreatitis. For example, hereditary pancreatitis is a rare genetic disorder that can cause recurrent episodes of pancreatitis, often starting in childhood. Other genetic conditions, such as cystic fibrosis, can also increase the risk of pancreatitis by causing thick, sticky secretions that can clog the pancreatic ducts.
High Triglycerides
High levels of triglycerides, a type of fat found in the blood, can cause pancreatitis. Extremely high triglyceride levels can cause the blood to become thick and syrupy, which can lead to inflammation of the pancreas. This condition is known as hypertriglyceridemia-induced pancreatitis.
Certain Medications
Some medications have been linked to an increased risk of pancreatitis. These include certain antibiotics, anti-inflammatory medications, and medications used to treat cancer and HIV. The exact mechanism by which these medications cause pancreatitis is not fully understood, but it is believed that they may cause inflammation or damage to the pancreas.
Infections
Infections, such as viral infections like mumps, can cause pancreatitis. The mumps virus, in particular, is known to cause pancreatitis in some cases, although this is relatively rare.
Trauma
Physical trauma to the abdomen, such as from a car accident, can cause pancreatitis by damaging the pancreas.
Tumors
Tumors, either benign or malignant, can block the pancreatic duct and cause pancreatitis.
Autoimmune Disorders
In some cases, the immune system can mistakenly attack the pancreas, leading to inflammation and pancreatitis. This is known as autoimmune pancreatitis.
Idiopathic Causes
In some cases, the cause of pancreatitis remains unknown, and this is referred to as idiopathic pancreatitis.
Symptoms and Diagnosis
Recognizing the symptoms of pancreatitis is crucial for early diagnosis and treatment. Symptoms can include severe abdominal pain that radiates to the back, nausea, vomiting, fever, and rapid heart rate. Diagnosis involves a combination of physical examination, blood tests to check for elevated pancreatic enzymes, and imaging tests such as CT scans or ultrasound to visualize the pancreas.
Treatment and Management
Treatment for pancreatitis depends on the cause and severity of the condition but often involves hospitalization for pain management, fluid replacement, and nutritional support. In cases where gallstones are the cause, surgery may be necessary to remove the gallbladder. For alcohol-induced pancreatitis, cessation of alcohol consumption is essential. Managing pancreatitis also involves treating any underlying conditions, such as high triglycerides or autoimmune disorders, and avoiding medications that can exacerbate the condition.
Prevention
Prevention strategies for pancreatitis include maintaining a healthy diet, avoiding excessive alcohol consumption, managing cholesterol and triglyceride levels, and avoiding smoking. Regular check-ups with a healthcare provider can help identify risk factors early on, allowing for timely intervention.
Future Directions
Research into the causes and treatment of pancreatitis is ongoing. Advances in genetic testing may help identify individuals at risk of hereditary pancreatitis, allowing for early preventive measures. Additionally, new medications and therapies aimed at reducing inflammation and promoting healing of the pancreas are being developed.
FAQ Section
What are the common symptoms of pancreatitis?
+Common symptoms include severe abdominal pain that radiates to the back, nausea, vomiting, fever, and rapid heart rate. These symptoms can range from mild to severe and require immediate medical attention if they persist or worsen.
Can pancreatitis be prevented?
+While not all cases of pancreatitis can be prevented, certain risk factors can be managed to reduce the likelihood of developing the condition. These include avoiding excessive alcohol consumption, maintaining a healthy diet, managing cholesterol and triglyceride levels, and avoiding smoking.
What is the difference between acute and chronic pancreatitis?
+Acute pancreatitis is a sudden inflammation of the pancreas that can be severe but is typically reversible with treatment. Chronic pancreatitis, on the other hand, is a long-standing inflammation of the pancreas that can lead to permanent damage and scarring of the pancreas, affecting its ability to function normally.
In conclusion, pancreatitis is a complex condition with multiple causes, ranging from gallstones and alcohol consumption to genetic factors and high triglycerides. Understanding these causes is essential for prevention, early diagnosis, and effective treatment. By addressing the underlying causes and managing symptoms, individuals can work towards healing and preventing future episodes of pancreatitis.